Heel Pain ICD-9 719.47 Heel Spur ICD-9 726.73
Heel Spurs – Self Help Tips, Treatment and Prevention From The Barefoot Running Doctor at Team Doctors
Tips For Better Health
Ask the doctor, Dr. James Stoxen DC
In this article is everything you ever wanted to know about Heel Spurs and more!
Do you think you have a Heel Spur because you have Heel Pain?
Does a heel spur even cause heel pain? Maybe the pain your having is plantar fasciitis?
What is a Heel Spur, Foot Spur or Calcaneal Spur?
A Heel Spur ICD-9 726.73 is a pointed bony outgrowth of the bone of the heel (the calcaneus bone). They are attributed to chronic local inflammation at the insertion of soft tissue tendons or fascia in the area. Heel spurs can be located at the back of the heel or under the heel, beneath the sole of the foot.
Heel spurs can occur alone or be related to underlying diseases that cause arthritis (inflammation of the joints), such as reactive arthritis (formerly called Reiter’s disease), ankylosing spondylitis, and diffuse idiopathic skeletal hyperostosis.
It is important to note that heel spurs may cause no symptoms at all. You might not recall any heel injury or trauma, which would have caused a bruised heel. and may be incidentally discovered during X-ray exams taken for other purposes.
Heel spurs are also called, foot spurs, bone spurs or a calcaneal spur, which in medical terms is a calcaneal exostosis, bone spurring of the heel or an osteophyte.
What are osteophytes?
Osteophytes take many months to years to form. You may feel no pain at all in the beginning and all of a sudden you wake up and say “my heel hurts”!
What are the symptoms of a heel spur?
Heel spurs start as a pain on the inside of the foot at the sole of the foot in the media aspect of the base of the heel.
It usually starts in the morning as sharp pains in the heel with the first few steps, which feel like someone is stabbing your heel.
As the day goes on usually the pain eases up to be just a sore heel pain.
They are associated with plantar fasciitis (plantar fascia is the connective tissue from the ball of the foot to the heel but can occur alone.
They are found mostly in middle-aged women and men but are common in younger people as well.
Few people get plantar fasciitis under 25 but more lately have been getting this condition.
I feel the reason for this is because footwear design is towards softer materials, which lack support. People are carrying more weight on their feet (overweight or obese) and most do not get enough of the right exercises.
How do you diagnose heel spurs?
When you present to the doctor pain in the bottom of the heel, there are a number of conditions this could be, such as:
- Plantar fasciitis– This is usually pain which is worse in the morning and commonly felt after prolonged sitting or standing
- Plantar fascia rupture – When the plantar fascia ruptures you will notice a fairly noticeable drop in your arch on that side with the over rolling of the foot in pronation
- Heel pad atrophy –The heel fat pad has some role in shock-absorbing on the landings with each step. How much of a roll has not been determined however some feel that the loss of thickness of the heel pad have can be a source of heel pain.” I really have never seen this to be the cause in any one of my patients with heel pain.
- Tarsal tunnel syndrome – this is different from heel spurs or heel pain as it is accompanied by pain, numbness or tingling in the heel radiating ONLY into the foot. If numbness is above the ankle it is coming from somewhere else above.
- Neuroma – This growth should be diagnosed with MRI.
- Bone cyst – This cyst of the heel should be diagnosed with x ray and or MRI.
- Osteomyelitis – This infection of the bone should be diagnosed with x ray and or MRI.
- Heel Fracture – This should be diagnosed with x ray and or MRI.
- Stress fracture(s) This should be diagnosed with x ray, bone scan or MRI.
- Tumor – This should be diagnosed with x ray and or MRI.
The diagnosis is made with an x ray of the heel spur from the side or a lateral film. 
However, just because your doctor sees the obvious spur, it does not mean the spur is the cause of your pain. Remember, spurs take years to develop so if your heel pain is recent (even months old) then the spur is only evidence that inflammation has been in the area for a long time but not necessarily the reason for your heel pain.
Just because the doctor sees no spur on the x ray around a painful and inflamed heel does not stop doctors from calling it heel spur syndrome. I don’t call it heel spur syndrome unless there is a heel spur on the x ray but every doctor is different.
Doctors feel that this osteophyte formation is a calcium deposit, build up on the heel bone from tissue around the heel stretching.
The heel spur or osteophyte does not cause the pain. In fact, over 50% of heel spurs are painless.
When the area around the heel spur is under abnormal stress it becomes inflamed causing heel pain or calcaneus pain.
Heel pain leads to them walking on the balls of the foot. When you walk on the balls of the feet to compensate it causes more pain because it pulls the fascia aggravating the plantar fasciitis more leading to more inflammation and calcium deposits on the spur.
How do you know how old a spur is?
The size of the spur can determine how old it is.
Then we can determine better when the spur started to form and that sometimes leads us to what caused the spur. This is easier in an area of the neck or lower back.
When I started reviewing x rays of the neck, lower back, shoulders etc, I would see calcium spurs in the spine of various sizes.
Then I would ask the patient “Did you have an auto accident, whiplash, sports injury or fall in your past where you ended up with neck pain?
Over the years I noticed that the older the injury the larger the spur. Soon I was able to predict within a few years when the patient had their injury based on the size of the spur.
A heel spur is different from arthritis spurs in that the spur does not form around a joint.
Heel spurs are NOT the cause of the heel pain!
I have never seen a case where the spur was the cause of the pain. We know this because after a few weeks the patient is pain free for 6-10 weeks of active rehabilitation but the spur is still there.
Spurs do not cause pain. They just tell you how long the area has been inflamed.
Evidence of this is with thousands of patients we note with back spurring, osteophytes or back spurs found on x-rays in areas that have not had pain in twenty years. You ask them if they had an injury 20 years ago and they can reflect on the exact injury.
Commonly they got relief and it had not hurt for 19 years then the area got aggravated recently prompting the visit to our center and the medical necessity for the x rays.
When you consult the American Podiatric Medical Association, they say that heel spurs are caused by strain on the muscles and ligaments of the foot and by stretching of the plantar fascia, which is a fibrous band of tissue that connects the heel and the ball of the foot.
It is normal for the body to lay down scar tissue, which calcifies. In a protective response, on the heel bone where it attaches to the plantar fascia.
We have to understand why spurs develop and that will lead us to the cause.
Spurs develop when the body tries to protect or repair itself. From pressure, pulling, rubbing or stress over years of abnormal motion.
What causes the spur to form?
This is still up for debate.
Without the obvious heel injuries it is hard for many to understand why the heel hurts. Without trauma, it is sometimes difficult for the doctor to understand why your heel hurts too.
So, x-rays are taken to determine why a patient has pain symptoms in the heel at the sole of the foot or a swollen foot and that is when the doctor detects the heel spur.
People think the pain comes from the sharp spur digging into the fascia but this is a misunderstanding.
It is estimated that 70% of patients with plantar fasciitis who do have discomfort will also be found to have a heel spur when observed via x-rays.
The spurs look sharp on the side x ray but the pain does not come from the spur stabbing the tissue. It comes from the stress on the heel.
- Where the plantar fascia, tendons of the foot, or ligaments of the foot are too tight
- Some doctors feel it is from tiny stress fractures in the base of the heel.
What are the risk factors for heel spurs?
- Shoe selection – You have a history or wearing high heels which maintain the Achilles in the shortened position stressing the arch.
- Shoe selection – You have a history of wearing flip-flops or sandals that force you to dorsiflex the foot to prevent the flop or sandal from falling off your foot.
- Plantar spurs may be a more modern phenomena resulting from long periods of standing and excess weight. (1)
- Having weak feet and ankles – There are many causes of weakness that cause the foot to roll into over pronation.
- Being pregnant, overweight or obese – Too much weight for the feet and ankles to support.
Where is the plantar fascia and what does the plantar fascia do?
This fascia attaches to the three main points of the foot (the heel or calcaneus, first, second, third, fourth and fifth meta-tarsal heads) to form the arch. This fascia is key to allow you to step down, move the weight of your body across the foot and to push off when you step.
According to research, scientists feel it only holds up 14% of the weight of the arch. Obviously some other structures hold up the other 86% of the load of standing, walking and running. In my opinion since it is not a contracting structure I don’t think it holds any of the load. Since there are no contractile elements like the muscles it must work via elastic recoil like a trampoline.
I feel the fascia is like a safety net that catches the load when the spring suspension system muscles are not doing their job. That also explains what happens when you have severe plantar fasciitis and the doctor cuts the fascia, the arch falls.
The conditions doctors say increase tension on the plantar fascia are acquired flat feet (pes planus), high arch (pes cavus), stiff or locked ankle joints and a tight Achilles tendon.
So I guess only those with arches that aren’t too high or aren’t too low are less susceptible to these heel spurs. That seems like everyone, doesn’t it?
You know why I disagree with this theory. Telling a patient that because they have a high arch that is the reason for their heel spurs is a cop out for a thorough exam to determine the true cause.
Also if you have had high arches all your life why do you suddenly feel pain one day and it’s a heel spur?
This is what doctors who believe in the lever model feel is the cause of plantar fasciitis and heel spurs:
- Walking patterns that put abnormal stress on that area of the heel bone (I agree)
- Excess weight, obesity pregnancy (I agree)
- Standing on feet for long periods (I agree)
- Sudden increase in mileage (I agree)
- Sudden increase in speed of walking or running (I agree)
- Increasing age which decreases the plantar flexibility and fat pad (I disagree)
- Running on hard surfaces (I disagree)
- Inadequate flexibility of the Achilles muscle group (I disagree ) This is not the only muscle group to focus on)
- Shoes lacking arch support (I totally disagree)
What it could mean is that the abrupt bang of the foot on the ground may be the cause of degeneration of the attachment of the fascia to the bone.
These are the standard treatments recommended by doctors who agree with the lever model and my opinion of them.
Pain symptom treatment involves relieving what causes the inflammation that leads to the pain. Here are the standard treatments that you may be offered by your doctor.
- Rest the feet – Rest is necessary at times to reduce the stress to allow the area to heal. However if the reason why you have too much stress in your heel area is from a weakness in muscles and tendons that take the load off this area then too much rest makes them weaker.
- You could ice the area with an ice massage. I would recommend this to decrease inflammation and pain.
- Some doctors recommend over the counter anti-inflammatories. I don’t recommend these as they can have side effects with prolonged use. I would recommend fish oil, turmeric and other natural anti-inflammatories instead.
- Some doctors prescribe you anti-inflammatories. The reason why you need a prescription for these drugs is because they come with risks or side effects with prolonged use. We have good results without them so why take the risk.
Inflammation is the healing process for the stress that is damaging the tissue. Instead of slowing the healing process why aren’t you focusing on what is causing the damage to the tissue and correcting that?
- Some doctors just give patients an injection of cortisone for the pain around the heel spur. As you know cortisone has major side effects. Did you ever wonder why you are not recommended more than three shots in your lifetime? In the case of plantar fasciitis the negative reaction can be serious and make it worse. You could more easily rupture of plantar fascia causing the entire arch to collapse requiring pretty radical surgery.
- Some chiropractors, massage therapists, physical therapists and athletic trainers recommend deep tissue massage treatments. This will help but to get maximum medical benefit you MUST be specific with your application and location of the massage around the tibialis posterior, the muscles surrounding the first second and third metatarsal cuneiform joints (arch muscles) and the muscles above like the TFL, gluteus medius, adductors and other stiff sore spasmed muscles.
- Doctors and trainers recommend stretching exercises and specifically stretching the calf muscle thinking that the calf (Achilles tendon – gastrocnemius and soleus) is pulling the heel up causing more tension on the fascia.
What if the Achilles muscle and tendon complex is tight because it is overloaded because the muscles that normally work with the Achilles are not doing their job (tibialis posterior).
Science has found that the plantar fascia only provides 14% of the support of the arch. If the arch is under stress then there are other structures that provide the other 86% of the support to focus on
Therefore, if you only stretch the Achilles as your approach to releasing stress on your plantar fascia, its usually ineffective.
- Many doctors and trainers recommend shoes that are softer. They seem to think that the soft shoe will be like a pillow for the spur. We already know that it is NOT the spur that is causing the pain. The abnormal stress on the heel area is causing the pain. If the shoe is too soft it cannot prevent the over rolling of the foot into over pronation which is what most researchers feel is what causes most abnormal stress on the tissues of the foot and above.
- Some recommend taping the foot. We all know that when athletes play football they are taped before the game and then again at halftime because the sweat and movement weakens the support function of the tape. In fact many trainers think tape is only good for a half hour of rigorous activity. Are you going to keep replacing the tape every hour of the day?
- Doctors and trainers recommend shoe inserts or orthotics. Doesn’t it seem like the arch support-orthotic would actually inhibit the spring loading shock absorption you need to resist the impact force safely into the arch of your foot that would protect your fascia from stress?
- Some doctors and web sites recommend a night splint. Splints put a constant stress on tissues. Researchers found that constant stress on tissue leads to plastic deformity over time. Tissues like the stress to be on and off as in a healthy contraction of the muscle. Tissues respond to constant strain by plastic deformity. These splints are uncomfortable and the theory behind them goes against the laws of nature. I have never heard of a patient improving with these devices.
- Some surgeons do low-dose radiotherapy– A total of 502 patients treated between 1990 and 2002 with low-dose radiotherapy (RT) for painful heel spurs were analyzed for prognostic factors for long-term treatment success. Overall 8-year event-free probability was 60.9%. Overall low-dose RT is a very effective treatment in painful heel spurs. (3) Does this treatment address the cause of the additional damaging stress in the area of the heel? No
- Some doctors surgically remove the spurs. I really don’t know why they remove the spur when it is believed it is a sign of chronic inflammation but not the cause of chronic inflammation and pain. I guess they have some way to know that this is one of those rare instances where the spur must be removed. I have never recommended this procedure.
- Some surgeons recommend surgery called a plantar fascia release if the condition does not resolve when all else fails. Who knows what was done before the surgery to determine what ‘all else‘ is.
I’ve seen where the doctors gave up and did the fascia release after a few cortisone injections with little to no physical therapy and recommendations that would actually increase stress to the area rather than decrease it.
Why plantar fascia release could be a very bad idea?
Science has found that the plantar fascia could provide 14% of the strength to support the arch. We already know there isn’t enough support for the arch because we have too much stress on it. Why would you cut a structure that is assured to make the area even weaker? Plus, you will not be able to walk normally for a few months making the area even weaker.
My warning to you is that fascia release surgery, cutting the plantar fascia, leaves the arch of the foot with less support leaving it at risk to drop causing more complications not only in the foot but up all 7 floors of the spring.
The plantar fascia serves an important function!
Complete rupture or surgical release of the plantar fascia leads to a decrease in arch stiffness and a significant collapse of the longitudinal arch of the foot. By modeling it was predicted such conditions would result in a 17% increase in vertical displacement and a 15% increase in horizontal elongation of the foot when it was loaded at 683 newtons (154 lbf).[1] Surgical release also significantly increases both stress in the plantar ligaments and plantar pressures under the metatarsal heads. Although most of the figures mentioned above are from either cadaver studies or investigations using models, they highlight the relatively large load the plantar fascia is subjected to while contributing to the structural integrity of the foot.
The plantar fascia also has an important role in dynamic function during gait. It was found the plantar fascia continuously elongated during the contact phase of gait. It went through rapid elongation before and immediately after mid-stance, reaching a maximum of 9% to 12% elongation between mid-stance and toe-off. (2)
During this phase the plantar fascia behaves like a spring, which may assist in conserving energy. In addition, the plantar fascia has a critical role in normal mechanical function of the foot, contributing to the “windlass mechanism”. When the toes are dorsiflexed in the propulsive phase of gait, the plantar fascia becomes tense, resulting in elevation of the longitudinal arch and shortening of the foot (see 3A). One can liken this mechanism to a cable being wound around the drum of a windlass (see 3B); the plantar fascia being the cable, the metatarsal head the drum, and the handle, the proximal phalanx. Therefore, the plantar fascia has a number of roles, the most important of these including supporting the arch of the foot and contributing to the windlass mechanism.
- ^ G. A. Arangio, C. Chen and W. Kim (June 1997). “Effect of cutting the plantar fascia on mechanical properties of the foot”. Clinical orthopedics and related research (339): 227–231. PMID 9186224.
- ^ Amit Gefen (March 2003). “The in vivo elastic properties of the plantar fascia during the contact phase of walking”. Foot & ankle international 24 (3): 238–244. PMID 12793487.
There are too many things in these approaches that don’t add up.
First, can bone spurs go away?
Second, do I need surgery to remove the spur from my foot?
The answer to both of these questions is NO!
The spurs wont go away and because the spur is not the cause of the pain. We do not have to remove or dissolve them for your pain to go away.
The spur, itself, does not require treatment.
Many doctors say heel spurs come from a constant stress pulling on the fascia. This may be true but it doesn’t explain some unexplained mysteries of this stress on the fascia and how it creates bone spurring.
Also the approach to treatment may not be the ideal approach for you.
What is interesting is that doctors find these heel spurs mostly on the medial or inner portion of the attachment of the plantar fascia to the heel. If the entire plantar fascia was stressed the heel spur would span the inner (medial), central and outside (lateral) portions of the fascia attachment of the heel. (see illustration)
If the medial portion is more associated with the first, second and third toes then what is the connection between plantar fasciitis and these toes? This could solve part of the mystery why the spur is mostly in the medial area and allow us to be more specific with our treatment and prevention.
How The Human Spring Model Explains Plantar Fasciitis and Heel Spurs
In order to understand what I am proposing, we have to understand the body as a human spring vs a human lever.
We also have to understand two simple principles of the physics of materials specifically, human tissue to “get this.”
There is the school of thought that the body moves through a series of levers.
Then there is the model I developed, the Human Spring Model which says the body moves, recycles energy and protects itself as a giant integrated spring mechanism
This article will explain the differences the human spring and human lever model.
Many “lever model only” thinkers believe impacts will injur the body.
That is why they recommend cushioned shoes for all running activities.
First, I will agree with the human lever model school of thought that the abnormal impact stress is what leads to plantar fasciitis and heel spurs.
The key word is “abnormal” impact stress.
Normal impact stress is good for the body. We adapt to it and that is how we get stronger.
In fact, elite athletes and even students in grade schools are now doing high impact training to bolster explosive power by conditioning the body to react elastically.
They call it plyometrics and it’s employed at every training center in the world from the Olympic training center and currently the grade schools. I learned the principles of plyometrics from the father of modern plyometrics, Yuri Verkhoshansky, at the Central Institute of Physical Culture and Sports Sciences, in Moscow, USSR, in 1989, when I was 27 years old.
You can read about it in the Post Video Tutorial #3 – The Human Spring Approach – Developed From Studying Yuri Verkhoshansky Plyometrics Training In Moscow 1987-89, click to view
Why have we been brainwashed into thinking impacts are bad for us and why are we paying huge dollars for impact resistant soles for running shoes, orthotics, gel inserts etc?
If these impact resistant soles are required to protect you from impacts then how would you explain why this 50 year old doctor who stands on his feet all day, night and on the weekends, runs barefoot on solid concrete or asphalt for 6200 impacts (6.2 miles 10 K) of 560 pounds per impact routinely with no shin splints?
To understand why I run barefoot, click here
In fact, I run barefoot on hard surfaces to strengthen my human spring mechanism to be more capable of handling greater impact forces safely, resist aging and prepare my body for my later years.
Human spring model thinkers, believe impacts strengthen the body.
Watch the video above as Dr. Stoxen explains How the spring suspension system muscles help you spring off the ground!
In reality, impacts strengthen the spring as long as the spring is intact and can handle the force of the impact.
What causes the abnormal stress that leads to the heel spurs?
This is the key to eliminating them!
The reason why you have stress on your shin muscles and shin bone causing shin splints and stress fractures is because there is too much stress there.
Can we agree to that profound statement?
When I examine patients with plantar fasciitis and/or heel spurs the first thing I notice is the over pronation landing or a rolling from supination (outside of the foot) to pronation (inside of the foot)
What protects barefoot runners from impacts?
Its the same thing that protects shod runners!
______________________________________________________________________________________
Allow me to introduce you to your human spring.
What is the difference between an intact or locked spring?
- When your spring mechanism is intact, you spring off the ground.
- When your spring mechanism is locked, you bang into the ground!
The natural spring mechanism is integrated into all 7 floors of the human body.
Essentially, the human body is a giant spring with 7 floors of springs;
- The arch
- The subtalar joint
- The ankle mortise
- The knee
- The hip
- The spine
- The head-neck
________________________________________________________________________________________
The plantar fascia is a fibrous gristle-like tissue with three portions—medial (inside), central, and lateral (outside).
The plantar fascia contributes to support of arch of the foot by acting as a tie-rod, where it undergoes tension when the foot bears weight. One biomechanical model estimated it carries as much as 14% of the total load of the foot.
What provides the remaining 86% of the load of the foot?
There are two mechanisms that allow the body to function as a spring:
- The configuration of the arch with the 26 bones and the ligament attachments, which includes the plantar fascia.
- The spring suspension system which is composed of the muscles and tendons that attach on the under surface of the arch.
The human spring model states that the body is protected by a spring mechanism that can absorb high force impacts through positive adaptation (training).
This can be done through the combined training approach of the body as a lever mechanism through progressive resistance exercises of the spring suspension system and as a spring through spring training such as multi-direction running drills, jumping drills and/or plyometrics.
First we have to agree that impact stresses are good for the body as long as we have an intact spring mechanism.
When are they not? – when the forces are taken up by tissues and not the spring.
This would be the plantar fascia and specifically the inside portion of the fascia that attaches to the first 2 or 3 toes.
For your foot-human body to absorb the force of the landing must function via elastic deformity vs plastic deformity.
Don’t worry this is not complicated and in fact it’s a simple concept that will help you make sense of all this.
Elastic Deformity vs Plastic Deformity
Define elastic deformity
- The foot and body deforms it shape to accommodate the force of the impact into the spring mechanism
- While it is deforming its shape it is also storing energy in the elastic elements and the shape change
- Then when all forces are fully absorbed and the spring reaches maximum depth it begins its return to its EXACT ORIGINAL SHAPE. The ability to reform back to its EXACT ORIGINAL SHAPE is important because this is the key to being able to walk, run and perform sports for a lifetime
- As it fully reforms it fully releases the stored energy
- Elastic deformity of your body is how you recycle energy and maximum protection from impacts and the preservation of your joints for a lifetime
- If your spring is fully released of muscle tension and joint stiffness or locking, fully flexible, strong enough, to absorb the impact force with enough endurance enough to absorb the amount of impacts you are using then you achieve 3 things:
When you exercise with a healthy spring mechanism, you cannot get shin splints. In fact here are the benefits to living with an intact healthy spring.
- Each impact stress will make the spring stronger
- You are at maximum performance efficiency (using spring elastic elements vs muscle lever pushing elements)
Notice on this graph ELASTIC DEFORMITY vs PLASTIC DEFORMITY how there is a point the body gets to a yield point. The yield strength or yield point is defined in in engineering where the amount of stress or kind of stress on the material begins to deform it plastically (permanently)
Prior to the yield point the material will deform elastically (snap back) to its EXACT original shape when the applied stress is removed (When you toe off). Once the yield point is passed, some fraction of the deformation will be permanent and non-reversible. We call this aging.
- True elastic limit – Up to this amount of stress, stress is proportional to strain your human spring can handle without remodeling your tissues. This means below this level you don’t get enough stress to improve your tissue strength
- Elastic limit (yield strength training zone) – This point and up to the deformity is when your muscles, ligaments, tendons and bones reorganize into a stronger mechanism. This is the zone you want to train in.
- Yield point – This is when your tissues damage by a negative stress It is a negative plastic deformity permanent damage occurs with every step or impact – ligaments stretch, discs weaken and bulge, discs degenerate, scar tissue infests elastic elements and muscles, spurs form, bones bend (bunions), micro stress fractures, shins splint, muscles ligaments tendons strain or pull, things start to stiffen and hurt.
- Failure Strength – this is when bones break, discs instantly herniate, meniscus tears, ankles sprain, muscles rip, tendons avulse or tear, ligaments tear
What is a plastic deformity that results from stress that overloads the arch and plantar fascia that attaches around the heel?
A heel spur!
Spurs form as a natural process of repair from repeated abnormal stress or stress when the human spring is not functioning in elastic deformity state.
The body lays down extra calcium at the site of the stress deforming it permanently or causing a plastic deformity.
Here are the various impact forces of landings:
- Walking (1.25 x bodyweight)
- Jogging 1.25 – 3x bodyweight
- Running (3x bodyweight)
- Plyometrics (3-5x+ bodyweight)
If you want to avoid heel spur pain you must make sure your spring suspension muscles are strong enough to absorb the forces of the impacts at the speed you want to travel.
You will learn how to test for this in the post below;
Video Tutorial #12 Is Running Bad For Your Knees? How Does The Body Spring Back Safely From Impacts Of Running and Walking?, click here
Video Tutorial #28 Self-Tests & Exercises To Reduce Over Pronation and Over Supination From Impacts During Walking and Running. click here
Examining a Patient For Heel Spurs with The Human Spring Approach
I start my examination of the painful foot with an inspection of the patient’s foot while they are lying down.
Im looking for swelling in the foot, deformities such as bunions, calcium deposits, specifically above the metatarsal cuneiform joint of the first toe area, discoloration such as brown patches, bruises or cuts.
Then I ask the patient to come out to our gait evaluation walkway and I video tape them in a weight-bearing positions such as standing, walking at a normal pace, walking fast and for some, running speeds.
I review the walking pattern on the video on the computer by moving the video frame-by-frame discussing with them how the force of the impact and transfer of weight into the legs is accepted by the feet and legs.
When you observe your walk you can check for abnormal pronation from rolling too far from supination to pronation or if the foot lands in an over pronated position.
You can also check for other biomechanical irregularities. Observation of your foot while walking may allow you to understand obvious clues to why there is too much stress in your heel.
This may seem very difficult to understand but it is really not. That is because often times the painful foot moves far different from the non-painful foot on impact. Many patients pick up on the abnormal stressful landing before I even point it out.
When the foot strikes the ground all 33 joints must have full springiness, joint play and mobility. Any excessive movement, stiffness or locking of any one of these joints can lead to abnormal stress on the area.
After we evaluate your walk we go into the room and evaluate the motion of all 33 joints to see if any of them are stiff, locked or moving too much.
Here is what I have observed clinically in patients with plantar fasciitis and heel spurs:
What I find over and over with patients with painful heel spurs:
- A stiffness or locking of the inside portion of the first metatarsal cuneiform joint, the second and third metatarsal cuneiform joints or what I call the arch spring!
- A weakness in the middle spring suspension system muscle of the arch spring of the foot (the tibialis posterior muscle).
- The weakness of this middle spring suspension system muscle causes the foot to either roll too far out of the safe range into over pronation or it lands in the already over pronated position.
This bang of the foot with the medial portion locked is what I feel causes the plantar fascia structure to become inflamed with constant standing, walking and running.
The first recommendation I have for you is to take a careful look at your walking form and technique to see if there are any signs of weakness or locking in the human spring mechanism.
Make your video of you walking towards and away from the camera for 10 feet or so at a normal walking pace then a second pass at the fastest walking pace you can do without running.
Watch it back advancing the movie slowly frame by frame. What do we see?
- Tension On The Arch And Limb On Impact – Are your feet, shins and legs relaxed prior and during impact? At impact and while transferring the weight across the planted foot are any of your toes pulled back before impact or after impact are any of the toes not touching the ground? Does your calf shake when it hits the ground (from the back)? Do you push or pull your body across the ground or spring your body off the ground?
- Foot Misalignment – Does your foot land with the second toe pointing the direction you are going?
- Foot/Heel Rolling Into an Unsafe Stressful Position Are your shin, ankle and foot in alignment or do you have weak or weak ankles? (Over pronation / over supination). Does your foot land in the already pronated position?
- Do you walk heel-toe or land heel first? There is no spring there. The impact goes bone (heel) to bone (talus) to bone (shin) the spring suspension system is in the middle/front of the foot!
What maintains the spring in the arch are:
- The spring suspension system muscles that support the arch mechanism as a sling from above and the intrinsic muscles of the foot that maintain the arch.
- The 26 bones and 33 joints and their connecting elastic ligaments that make up the arch configuration.
- The fascia – Remember that fascia does not have contractile elements. Therefore they are only stretched with the first and second line of defenses being the arch spring and the spring suspension system muscles have been exhausted.
Gait corrections
If you see any flaws in your walk or run then you MUST work on your walking and running form and technique.
#1 Tension On The Arch And Limb On Impact Use Mind Body Relaxation – prior to landing your foot, relax the muscles of the shin and the rest of the limb so that the impact can enter the spring mechanism of your body without internal compressive force on it from tension.
The lack of spring in the arch causes an abrupt impact, which may be the source of the stress that leads to the inflammation and pain in your heel. Because the spur is mostly found in the medial aspect of the plantar fascia it makes sense to unlock or loosen up the metatarsal cuneiform joints of metatarsal one, metatarsal two and metatarsal three.
What I have found is that fascia can be treated just like muscles and ligaments with deep tissue work. I recommend the deep tissue spring release techniques to release the muscle around the first second and third metatarsals as well as all the stretches of the foot
In younger people the plantar fascia is also intimately related to the Achilles tendon with a continuous facial connection between the two from the distal aspect of the Achilles to the origin of the plantar fascia at the calcaneal tubercle.
Nevertheless, there is an indirect relationship whereby if the toes are dorsiflexed the plantar fascia tightens via the windlass http://en.wikipedia.org/wiki/Windlass mechanism. If a tensile force is then generated in the Achilles tendon it will increase tensile strain in the plantar fascia.
Clinically, this relationship has been used as a basis for treatment for plantar fasciitis, with stretches and night stretch splinting being applied to the gastrocnemius/soleus muscle unit.
Just stretching one muscle all night or just stretching of the Achilles consisting of the gastrocnemius and soleus muscles and not all muscles around the three dimensional foot may actually put you at a higher risk for injury than lower.
The Academy of Sport Medicine has found that runners who do excessive stretching tend to have a higher incident of accidents. The reason for this is simple— muscles are like twine and not like a rubber band. That is that they twist open or shut and don’t stretch like rubber
Dr. Stoxen’s best stretches for Heel Spur video tutorials;
Video Tutorial #84 Dr James Stoxen DC Demonstrates Scissor Stretching Of The Feet
Video Tutorial #85 Dr James Stoxen DC Demonstrates Stretching Great For Morton’s Neuromas
Video Tutorial #88 Dr James Stoxen DC Demonstrates Stretching Of The Foot While Sitting
Video Tutorial #89 Dr James Stoxen DC Demonstrates A Stretch To Increase The Arch
Don’t do too much stretching of the wrong muscles such as the Achilles. Remember the foot is a three dimensional springy platform so you MUST stretch the foot in all directions to make sure it is as flexible as possible to comfortably absorb the force of the impact without abnormal stress on the fascia.
View the links below to Dr. Stoxen’s self help video tutorials for Heel Spurs;
Video Tutorial #78 Deep Tissue Treatment Of The Knee Popliteus Muscle
Video Tutorial #79 Deep Tissue Treatment Of The Gluteus Medius Muscle of the Hip
Video Tutorial #80 Deep Tissue Treatment Of The Subtalar Joint Of The Ankle On The Inside
Video Tutorial #81 Deep Tissue Treatment Of The Ankle (Subtalar Joint Outside)
Video Tutorial #82 Deep Tissue Treatment Under
Video Tutorial #83 Deep Tissue Treatment Above
Video Tutorial #87 Deep Tissue Of The Ankle Mortise
#2 Foot Misalignment – Practice walking with the foot landing with the second to pointing towards the target.
#3 Foot/Heel Rolling Into an Unsafe Stressful Position – Any weakness in the spring suspension system- Make sure the spring suspension system muscles are strong enough to support the force of the loading directly on them and strong enough to maintain the foot in the safe range between supination and pronation.
If your muscles are not strong enough to maintain the foot in the safe range you cannot strengthen them overnight so it’s strong enough to keep the foot in the safe range. For some of you it would take months and for some of you it means a combination of losing a lot of weight and a lot of training. Either way we need to keep the foot in the safe range without putting something in the way of the natural spring mechanism like an arch support or orthotic.
What are the best Shoes for Heel Spurs / Shoes for Heel Pain?
My solution is a shoe that has an extended medial counter support to maintain the heel in the safe range. Because the arch is an interconnecting mechanism of bones and elastic ligaments and because you have already released all the spasms around it, it should spring up and down now without abnormal stress on the heel and fascia. The trick is to just maintain the foot in the safe range and this shoe design does that.
#4 How do we correct the form and technique of your walk
- Land with foot-leg-hip directly more perpendicular to earth gravity and body
- When you are perpendicular to the pull of gravity is when your spring should be loaded at full depth.
- It shouldn’t be when you hit your heel first
Regardless, it is impossible to walk or run with perfect stress free form and technique without all restrictions removed from the spring and for it to be strong enough to handle the impact forces of movement at the speed you want to travel, walking, jogging, running and/or plyometrics.
#5 Heel Spur Preventive Exercises – You must develop the spring suspension system muscles to support the arch so there is not a lot of load dumped on the plantar fascia.
This requires you to:
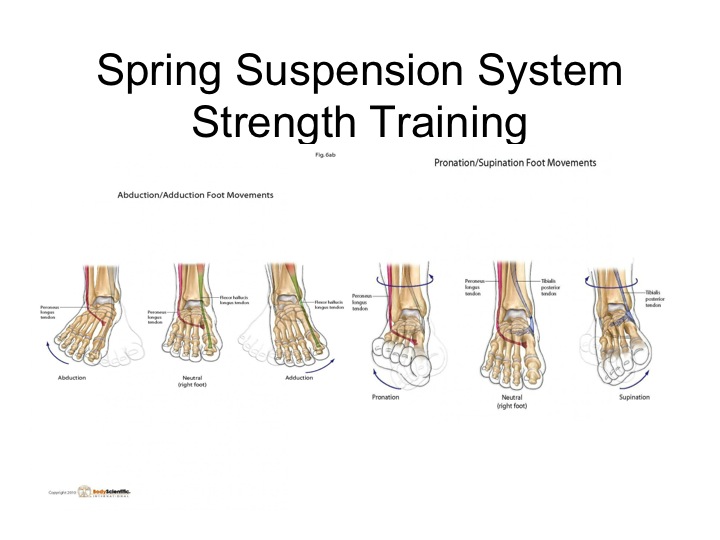
SPRING RESISTANCE TRAINING– Strengthen the spring suspension system muscles like a lever. Train with resistance exercises adding cuffs strapped to the foot moving it in a variety of directions such as eversion, inversion, abduction, adduction, pronation and supination.
SPRING IMPACT TRAINING – Strengthen the spring like a spring. I restore the spring suspension system muscles ability to resist impacts with barefoot drills like zigzag patterns, circular patterns, shuffle patterns as well as doing multi direction plyometric drills with graduated increased speeds starting with walking, jogging, running plyometrics.
Because we are going to release our natural spring mechanism, artificial spring protection like heavy cushioned soles wont is necessary. In fact, we should set a goal to get back to walking and running barefoot like we did as a youth.
Why?
“The inability to walk or run barefoot safely is one of the first signs of aging “
Are we running to slow the aging process or speed it up?
Then when you’re in the competition you can cheat by putting shoes on that allow for additional recoil of the elastic of the shoe!
Can I still run with painful heel spurs?
NO WAY!
Can I walk or run with non-painful heel spurs?
Of course!
How do you know when it is safe to run again?
You just don’t go out and run and see what happens!
You have to videotape yourself walking, jogging and running at increased speeds, which test the impact resistance of the spring suspension system to maintain the foot and limb in the safe range.
Watch this video below of national champion taekwondo, Christian Medina and Dr. Stoxen running barefoot down the street. One of our staff was in the back of an SUV videotaping through the window while another staff member was driving.
These are the snapshots taken from the video analysis.
As you can see we ran the entire run in zig-zag patterns. This forces the foot to land in positions that naturally release the 33 joints from different angles and strengthens the suspension system muscles equally from the inside and the outside.
That is how I have been able to run barefoot on solid concrete and asphalt streets without Thoracic Outlet Syndrome, Heel Spurs, Morton’s Neuromas, shin splints, or other impact related conditions.
You would think that running and jumping as in plyometrics would make one more susceptible to heel spurs due to the stresses of the landings. This is only true if you have a weak, stiff or locked spring mechanism at the time of the training.
Joint subjected to heavy impact are relatively free from osteoarthritis in old age and that those subjected to much lower loading experience a greater incidence of osteoarthritis and cartilage fibrillation (5) (6)
Conclusion
There is no one perfect approach. However, we should approach to heel spurs and other conditions with logic that follows the laws of physics and nature.
I have tried my best to present to you my best recommendations based on these laws, the prevailing scientific literature and my many years of clinical experience.
You may not rush off to your family chiropractor or alternative medical center for this but I have found that conservative treatment at our chiropractic center with an integrative medical approach.
Please feel free to share your Heel Spur story in complete anonymity in the comments below. I will advise the best I can.
Thank you for sharing this article with those you feel it can help!
Research Articles
1. Weiss E. Calcaneal spurs: examining etiology using prehistoric skeletal remains to understand present day heel pain. Foot (Edinb)2012 Sep;22(3):125-9. doi: 10.1016/j.foot.2012.04.003. Epub 2012 May 3. [PUB MED]
2. Li J, Muehleman C. Anatomic relationship of heel spur to surrounding soft tissues: greater variability than previously reported. Clin Anat. 2007 Nov;20(8):950-5. [PUB MED]
3. Muecke R, Micke O, Reichl B, Heyder R, Prott FJ, Seegenschmiedt MH, Glatzel M, Schneider O, Schäfer U, Kundt G. Demographic, clinical and treatment related predictors for event-free probability following low-dose radiotherapy for painful heel spurs – a retrospective multicenter study of 502 patients. Acta Oncol. 2007;46(2):239-46. [PUB MED]
4. Kumai T, Benjamin M. Heel spur formation and the subcalcaneal enthesis of the plantar fascia. J Rheumatol. 2002 Sep;29(9):1957-64.
5. Tweed JL, Barnes MR, Allen MJ, Campbell JA. Biomechanical consequences of total plantar fasciotomy: a review of the literature. J Am Podiatr Med Assoc. 2009 Sep-Oct;99(5):422-30.
Disclaimer
All content on teamdoctorsblog.com, including without limitation text, graphics, images, advertisements, videos, and links (“Content”) are for informational purposes only. The Content is not intended to be a substitute for professional medical treatment, advice, or diagnosis. Please remember to always seek the advice of a qualified physician or health professional with any questions you may have regarding any medical concerns. Dr James Stoxen DC and Team Doctors does not recommend or endorse any specific treatments, physicians, products, opinions, research, tests, or other information it mentions. Said Content is also not intended to be a substitute for professional legal or financial advice. Reliance on any information provided by Team Doctors is solely at your own risk.