Stress Fracture (2nd Metatarsal) ICD-9 829.0
Stress Fracture (2nd Metatarsal) ICD-9 829.0
Stress Fracture Of the Second Metatarsal – Self Help Tips to Treatment and Prevention from The Barefoot Running Doctor
Tips For Better Health
Ask the doctor, Dr James Stoxen DC
With an increase in public interest in physical fitness, clinical practitioners are diagnosing stress fractures of the foot or metatarsal stress fractures with greater frequency. First described by Aristotle in 200 BC, stress fractures were initially recorded in the medical literature in 1855 by the Prussian military physician Breithaupt, who described what is now known as a march fracture, or stress fracture of the metatarsals.
The most common position for a metatarsal fracture is a second metatarsal fracture, especially in those whose second toe is longer than their big toe. It is also more common in those who overpronate with the first metatarsal in a dorsiflexed position as this places greater load on the 2nd metatarsal.
What is a stress fracture? Stress fractures or sometimes called micro fractures can occur from; Over use, Too much training, too soon, overpronation and oversupination. They are also common in army recruits (often called a march fracture), runners, ballet dancers and gymnasts.
In this post I will answer a question regarding a stress fracture of the second metatarsal from the barefoot runners society website.
You can read the forum thread by clicking here
Patient’s Question:
– I’m a long time runner but I am relatively new to minimalist running who is apparently having some transition issues (former stable/orthotics shoe person who fixed her gait/form and heal strike issues in a pt/medical environment).
– Transitioned Jan/Feb – in March I had some mild top of foot pain which didn’t hurt while running but did afterwards, no inflammation/bruising – expected it was tendonitis so I treated with ice and waited for no pain for a week and then started back running again. (Note: I was only up to about 5 miles in distance and ran about 3-5 times a week anywhere from 3-5 miles (trying to keep adding a bit more).
– About a week later I was on a 4.5 mile run and close to the end had pain/tightness in the opposite calf which remained for about a week (during which I iced, rolled, stretched).
– After about a week of no pain, I started to run again, and after a few days, the top of foot pain returned after a 4 mile run but it was much worse. Back to rest/icing – symptoms seemed to follow Extensor Tendonitis (vs. a stress fracture (comparing the symptoms of a SF I had a few years ago).
– Pain has reduced over the past 4 weeks, but still remains so I decided to get an x-ray to see if anything shows up. Primary Dr. just called to say indeed there are definite signs of a stress fracture in the mid-shaft around the 2nd toe/metatarsal (I don’t have the report yet but this is what was stated on the phone). She recommends going to a specialist to see how they want to treat.
– At this point, assuming it’s on its way healing and if I start wearing a “boot” am I good to go? Not discounting the specialist’s expertise, just based on my first experience, not clear if there is any more that they would do other than confirm the diagnosis and tell me to wear a boot for x number of weeks…Am I missing anything? THANKS!!!
Dr Stoxen’s Answer:
Stress Fracture – Mid Shaft/2nd Metatarsal – Regardless if you have a stress fracture or pain that feels like a stress fracture or not, you have too much stress on the second metatarsal. That is why its called a ‘stress fracture.’
That’s why you have a stress fracture of the second metatarsal, if in fact you really have a stress fracture. That has not been determined yet.
The key to this is not whether or not you have a stress fracture but why you have a stress fracture or too much stress in this area. That’s what we have to figure out and eliminate so that you can go back to running barefoot for life.
The body and specifically the foot has ingenious ways of absorbing or springing off stressful impacts. Stress is actually good for the body because stress allows the body to be stimulated to adapt to get stronger.
When is stress not good for the body? 
- When stress is abnormally applied to the joints from poor form and technique.
- If the joints are locked not allowing the impact to be absorbed into a movable joint.
- If the muscles that attach on this particular joint are not strong enough to absorb the negative impact loading from that impact landing.
Just like a plane, the human body has a landing gear, spring-loaded shock absorbing mechanism built into the arch complex as well as the muscles that allow the dissent of the foot during impact like descending weights during a bench press or curl.
The human foot has 33 joints that allow 26 bones to move freely during impacts such as walking and running and other activities. The reason why it has 33 joints is because when you impact with the earth that impact can be spread across these 33 joints lessening the overall impact on any one area.
So why do you have more stress on the second metatarsal than on the other 26 bones of your foot?
If all the foot joints are moving the way they should be, then like I said, the stress will be distributed among the joints smoothly and you should be able to run without any problem. Obviously there’s a problem with the distribution of stress otherwise you wouldn’t have a stress fracture or too much stress on the area.
Here’s what I see that happens over and over again clinically in my chiropractic practice that might help you understand what could be happening.
When the human body impacts the ground, the entire human spring mechanism absorbs the impact through the floors of the entire body, the foot, the ankle, knee, hip, spine etc. Specifically the initial impact at the foot is absorbed through two mechanisms:
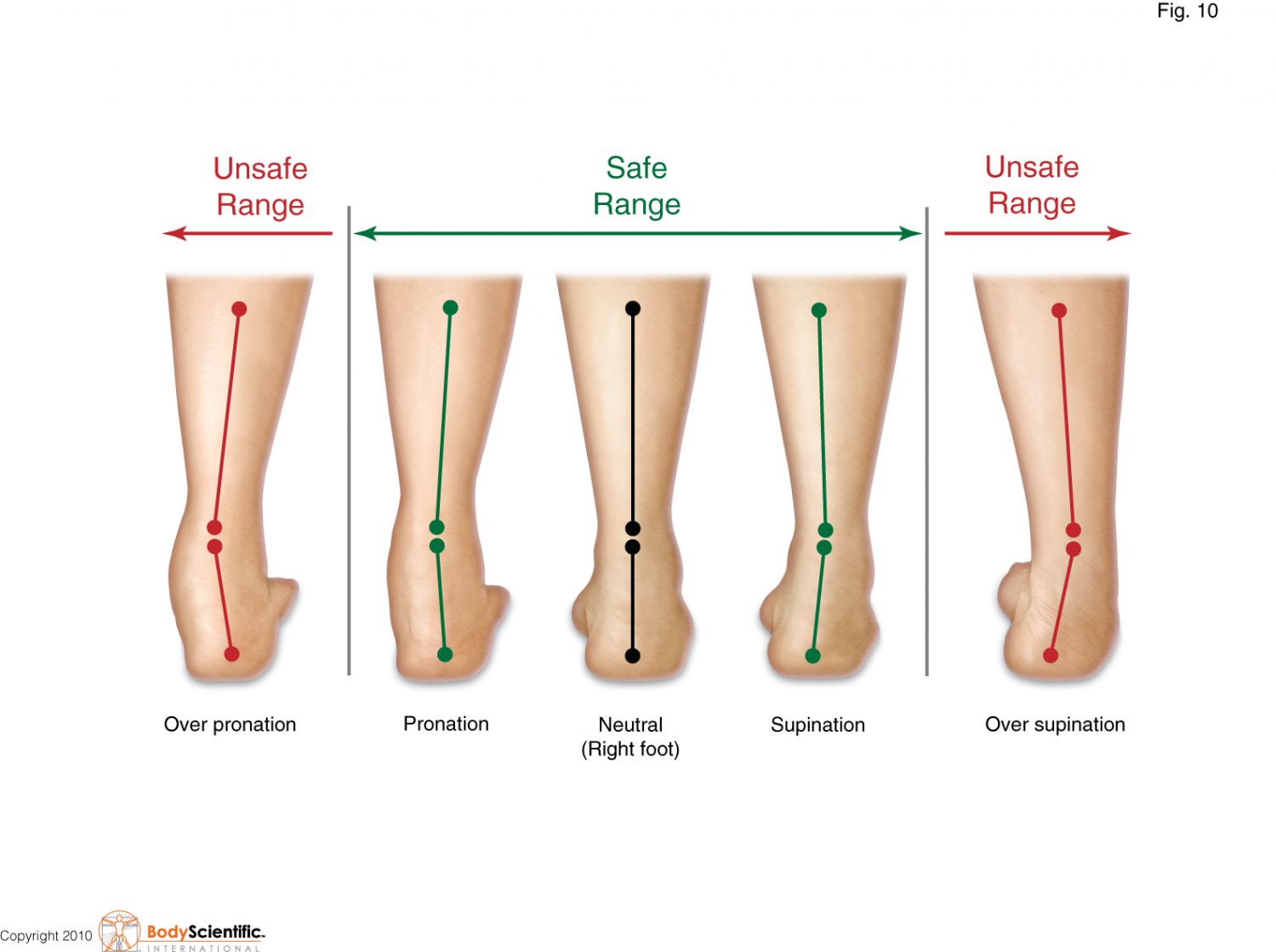
The foot rolls from the outside to the inside. This is the rolling from supination to pronation. This rolling occurs as the force of the impact is gradually loaded into the foot along a particular path that loads it the safest. It obviously loads differently for all kinds of impacts. For instance if you’re doing a side shuffle drill, zigzag runs, hops, skips, lunges etc.
However, the foot has loading muscles. This is like loading the impact of the weight of the dumbbells as a negative in the bench press. Some muscles of the foot stretch and load the impact into them and when the foot hits the bottom, it points and goes into the toe off and snaps the foot back into its original position.
Pronator Supinator Cuff AKA Arch Sling, Arch Spring Cuff; The Spring Cuff Or The Spring Suspension System
This is what I call the human spring.
The ability to load this impact follows the laws of physics in particular Hooke’s law.
To learn more about The Human Spring Approach In It’s Relationship To Hooke’s Law Of Physics read video tutorial #9, click here
Certain activities can sabotage this event. For instance if you are holding a book in your hand with your arm in a 90° angle for 30 minutes (like a curl) the bicep muscle tightens and stiffens and you will not be able to hold it very much longer perhaps because of the pain and stiffness in the joint of the elbow.
You might have to do deep tissue work around the muscles of the elbow to get the elbow joint to free itself up again. (see below in the post for information on how to do the self help, deep tissue releases)
Foot swelling:
Is there foot swelling? If so, ice it and it should heal up. If it does not after several days of self help treatment in this article you should see a doctor and get an x-ray.
Foot Lock:
The same thing happens to the spring suspension system muscles, the negative loading muscles of the foot spring suspension system. You might not find this lingo in books because I made it up, to be able to explain this in easier terms for the public to understand. If I explained it to you in mechanical/medical terms you might have stopped reading this article a long time ago.
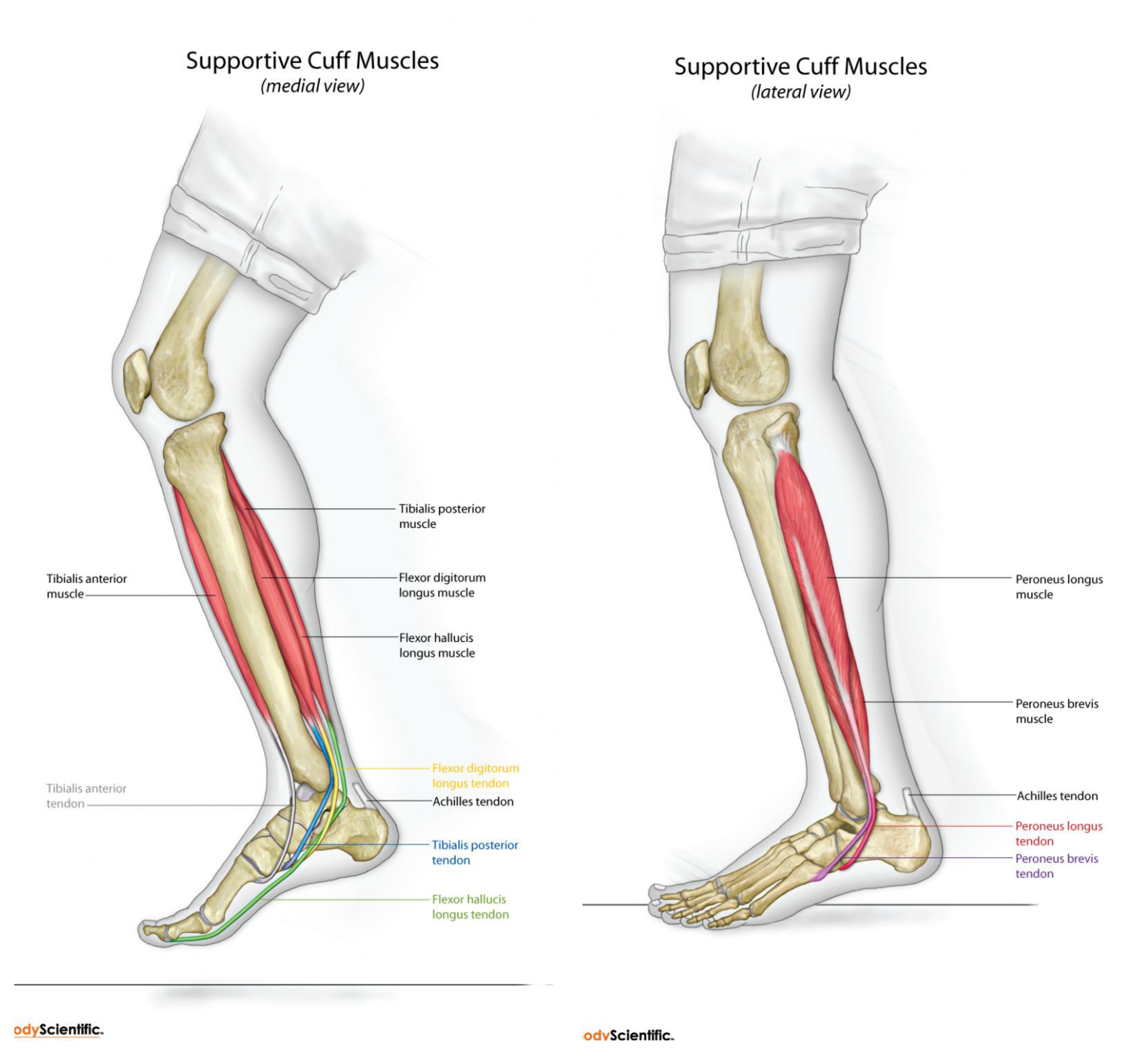
So if you stand on your feet for a long period of time or on that particular foot for longer than you should, any one of the muscles, such as the tibialis posterior, anterior or peroneal muscles get tired, fatigued causing the complex to drop in the mid-arch complex to lock. What I have found clinically is it locks the majority of the time at the second metatarsal-cuneiform joints and sometimes the third metatarsal-cuneiform joints.
To learn more about Foot Lock! What You Get From Standing Too Long And How To Prevent It read video tutorial #159, click here
To check for this we do what we call motion palpation of the joint play in that joint complex which is around your mid arch. see video below;
A more fun way of describing it is called the wiggle test. Get a grip on your mid foot and a grip on your second metatarsal, the second long ball of your foot and wiggle those two back and forth to see if there’s good joint play. What you might find is that it’s stiff as if it’s been in the freezer for a while similar to what chicken feels like when you’re pulling it out of the freezer the joints are frozen. If you exceed the maximum amount of force that the spring mechanism can load it’s called failure strength and that’s how you get the stress fracture.
If you release as many joints in your foot as you can then you can spread the force out across all the other joints and keep the stress off your second metatarsal in the future.
In fact there is a tendon from the tibialis posterior that attaches directly on the second metatarsal in that area of your stress fracture. If the tibialis posterior is really tight and doesn’t let the second metatarsal spread on impact it could be stressing that bone on impact. (see image below) The attachment of the tibialis tendon to the second metatarsal is in blue)
After you do that you can take your thumb and stick it into the point of the second metatarsal joint at the soul of your foot and see if there is pain there. A stress fracture isn’t a fracture that’s broken through. So you can push on the bone and it won’t fracture further. If you can run on it, that’s about 300 pounds of force on the foot. You can’t possibly develop the kind of force with your thumb print into that area. Also the doctor said it wasn’t fractured, so I would not be afraid to do this.
How do you treat stress fractures of the foot? By applying the pressure to this muscle you can release the spasm that restricts the movement of that joint. If you start at the base of the heel and apply these deep tissue pressure points one thumbprint at a time to the knuckle of the second metatarsal you can release the muscle spasm that is restricting the second metatarsal cuneiform joint from moving.
The video tutorials below will show you how to do this deep tissue treatment:
Video Tutorial #82 Deep Tissue Treatment Under The Big Toe And Second Toe
Video Tutorial #83 Deep Tissue Treatment Above The Big Toe And Second Toe
Video Tutorial #84 Scissor Stretching Of The Feet
Throughout this entire rehab process you should be spending about a half hour to 40 minutes a day doing your own deep tissue on your foot, which includes your;
- Second metatarsal
- Third metatarsal
- First metatarsal sub scale or joint ankle mortise and
- The tibialis posterior muscle.
Check for Sub-Clinical Shin Splints too:
Note that the second metatarsal cuneiform joint is locked and your impacts are going to be more of a bang than a spring. Like I said if that joint is locked then it can’t flex two load the impact into the joint comfortably so that’s why you have distressed–fracture or stress causing pain. So if you can’t load the impact into that joint you might not be able to load the impact and the entire land, the majority of the weight is held by the first and second metatarsal’s. The third fourth and fifth just guide the foot while absorbing a minimal amount of impact force. In order for you to get this second and third metatarsal cuneiform joint to unlock, at the least you really have to wiggle it pretty good. You may hear a click when the joint releases. Just keep it loose and wiggle it back and forth to wiggle it lose.
To learn more about Video Tutorial #75 The Deep Tissue Treatment Dr. James Stoxen DC Uses For Shin Splints click here
Below you will find additional deep tissue techniques that you can use to release the complex 33 joints so that the stress of the impacts can be absorbed more comfortably across the joints rather than the majority of it through the second metatarsal.
Hopefully you will be back to running again without pain and this should help you with that.
Video Tutorial #77 How to Self Adjust Your Toes
Video Tutorial #78 Deep Tissue Treatment Of The Knee Popliteus Muscle
Video Tutorial #79 Deep Tissue Treatment Of The Gluteus Medius Muscle of the Hip
Video Tutorial #80 Deep Tissue Treatment Of The Subtalar Joint On The Inside
Video Tutorial #81 Deep Tissue Treatment Of The Subtalar Joint Outside
Video Tutorial #85 Great Stretch For Mortons Neuromas And Narrow Heels
Video Tutorial #87 Deep Tissue Of The Ankle Mortise
Video Tutorial #88 Stretching Of The Foot While Sitting At Your Chair
Video Tutorial #89 A Stretch To Increase The Flexibility Of The Arch Of Your Foot
If you would like to consult with Dr Stoxen by phone about any condition, please call 773-735 -5200. There are no charges for phone consultations.
Like this article? We will send the next one to you.
Register for our updates below:
Disclaimer
All content on teamdoctorsblog.com, including without limitation text, graphics, images, advertisements, videos, and links (“Content”) are for informational purposes only. The Content is not intended to be a substitute for professional medical treatment, advice, or diagnosis. Please remember to always seek the advice of a qualified physician or health professional with any questions you may have regarding any medical concerns. Dr James Stoxen DC and Team Doctors does not recommend or endorse any specific treatments, physicians, products, opinions, research, tests, or other information it mentions. Said Content is also not intended to be a substitute for professional legal or financial advice. Reliance on any information provided by Team Doctors is solely at your own risk.