Morton’s Metatarsalgia ICD-9 355.6
Morton’s Neuroma – Self Help Tips, Treatment and Prevention From The Barefoot Running Doctor at Team Doctors
Tips For Better Health
Ask the doctor, Dr. James Stoxen DC
In this article is everything you ever wanted to know about Morton’s neuroma and more!
Is your foot hurting?
Do you have tingling in the feet or burning feet?
Do you have foot aches and do you have toe numbness?
The “Morton’s Metatarsalgia ICD-9 355.6” (pain between the toes) was first observed in 1835 by Filippo Civinini (1805-1844) (1)
Morton’s neuroma is a common cause of metatarsal swelling and pain – on the bottom of the foot that radiates from between the third and fourth metatarsals, which may cause extreme pain and disability.
Morton’s neuroma, also known as Mortons toe, is one of the most common disorders encountered in the foot (2) and a common cause of metatarsalgia or pain between the third and fourth toes. (3)
Although Morton neuroma is a common diagnosis, debate exists as to the best surgical and nonsurgical treatments. This article discusses the cause, how to diagnose it, nonsurgical and surgical management, and surgical complications of Morton’s neuroma (4) as well as how to avoid it.
What is a Morton’s Neuroma?
Most neuromas, 53%, are located in between the third and fourth toes (metatarsal heads) where the branches of the medial and lateral plantar nerves join. (2) However, neuromas have been found in between the second metatarsal bone and third metatarsal bones in 25% and 22% between the fourth and fifth toes. (2)
The fibrous neuroma develops when the area around the nerve is inflamed and heals itself with scar tissue, which leads to an enlargement of the nerve. This enlargement gets compressed with every step causing it to get bigger and bigger.
When it flares up, Morton’s neuroma creates a sensation of burning or sharp pain and numbness on the front part of the foot (forefoot). These symptoms radiate foot pain in the front of the foot.
“Why do my feet hurt?”
I did not have any injury so how did I get this?
Morton’s neuroma is different from a traumatic neuroma as it happens over time. It starts like a random common pain in the foot. People say, “The bottom of my foot hurts when I walk” They should say, “The bottom of my foot hurts when I walk in these pointy toe high heel shoes.
Why don’t men get it as often?
Morton’s Neuroma occurs more often in women than men, and particularly in those who wear narrow, high-heeled shoes. (5) Men do wear shoes that are too narrow but not on the same scale as the narrow pointed shoes that women wear, plus lifting the heel slides the foot down into this narrow point further squeezing the toes pinching the nerves.
Morton’s neuroma is not a true neuroma. A true neuroma is a tumor of nerves.
Morton’s Neuroma Diagnosis is instead a condition which, “consists of scar tissue and blood vessels that infiltrate the nerve fibers and cause further damage to the nerve and its covering” (6)
Aren’t Morton’s Neuroma Only For Middle Aged Women who wear high heel pointy-toed shoes? No!
The female-to-male ratio for Morton’s neuroma is 5:1 and up to 10:1 (7) however some as young as 15 have got them and men get them too.
How do you get Morton’s neuroma? What causes Morton’s neuroma?
Don’t all Morton’s neuroma’s hurt? Will I know when I have them?
No! You can be checked for the risk factors in a few minutes by a few easy tests and by watching yourself walk.
Then you can make the adjustments I recommend in this article to reduce the risk before your feet start swelling and you have pain.
If you know the cause of a condition you can treat and prevent it.
There could be several causes of a Morton’s neuroma. So, if you are looking for a magic cure, there is not one single remedy.
What are the causes of the Morton’s neuroma?
The neuroma pain is caused by over use stress and strain in the area that leads to the release of inflammation. When an area has chronic inflammation, it doesn’t necessarily cause a swollen foot, but over time, it leads to a constant layering of scar tissue in the area.
That is what doctors and scientists feel cause the neuroma.
Some doctors and scientists believe this abnormal over use stress comes from an abnormal or poor walking form such as overpronation (foot over rolls when it plants), the combination of hypo mobility and hyper mobility where the bones of the foot are both stiff or locked and others move excessively to make up for the locked ones, and of course the obvious, narrow or high heel shoes.
___________________________________________________________
You don’t have to have chronic pain in the area to have a constant layering of scar tissue. Only when the inflammation gets high enough do you have a swollen foot and feel pain. Inflammation can stay under the brains radar as “silent inflammation” or “low grade inflammation” but still over years do its damage. Inflammation in the foot can get pretty high without you feeling pain.
Some people have pain in their feet every day and think its normal. They don’t realize that part of the inflammatory process is the layering down of scar tissue. Chronic low grade inflammation increases the risk for many diseases of aging so don’t let this chronic foot pain go on.
For more information on the damaging effects of inflammation read these articles:
The Inflammation-Depression Connection Approach and The Science Based Natural Approach to Depression, click here
Video Tutorial #37 Aches, Pains, Allergies, Fatigue, Brain Fog, Diseases of Aging Have One Common Thread… INFLAMMATION, click here
Don’t wait until you have a painful swollen foot and a thick fibrous neuroma between your toes because then it is more difficult to treat.
__________________________________________________________________________________________
What is the standard examination in a doctor’s office to confirm a Morton’s neuroma?
Web Space Compression Tenderness Test – Doctors push their thumb between the 3rd and 4th toes (metatarsals). If there is pain there they suspect a Morton’s neuroma.
Foot Squeeze Test – Doctors squeeze the foot from the sides and if it hurts between the bones, they suspect a Morton’s neuroma. (8)
Gauthers Test – involves squeezing the metatarsals together and moving them up and down for 30 seconds, which leads to pain.
__________________________________________________________________________________________
Morton’s Neuroma Diagnosis
How do I know it’s not a foot stress fracture?
The Morton’s pain and foot symptoms are different from a foot stress fracture symptoms in that it feels like there is a ball or stone in the bones of the foot. Patients feel as if they have a bruise causing pain and swelling under the third or fourth toe or line a stone impact bruise where the bottom of the foot hurts between the second metatarsal bone and third metatarsal bone but primarily between the third toe and fourth toe and knuckle joints of the toes.
What else could this pain be?
With such a limited physical examination, doctors are unable to rule out other conditions that may be causing the pain. This might be a stress fracture of the neck of the metatarsal, a neoplasm or cancer, Freiburg osteochondrosis, ganglion cysts, a true neuroma, a neurofibroma, a schwannoma or a locked and misaligned, metatarsal.
The foot has 33 joints to absorb the impact forces of over 3,500,000 impacts or steps from walking or running per year. If one or two toes are locked other toes may have to move excessively to take up the impact forces. It is important for doctors to check for these abnormal movement patterns of the toes to see if this is the cause of a Morton’s neuroma.
In my office I find most patients have a locked and misaligned metatarsal, which is part of a more complex locking of many bones of the foot. Read on…
Because most doctors do not check for joint play or abnormal movement patterns in the 33 joints of the foot a lot of them miss this. Also because doctors are not taught how to manipulate the foot they wouldn’t think to look for it.
You check for locked or excessively moving bones in the foot with the foot wiggle test. It wasn’t invented by one of the Wiggles but I have checked the Wiggles with this test.
Morton’s Neuroma Vs Metatarsalgia – Diagnostic Tests Diagnostics
Diagnostic Imaging
The first step is to make sure you have a Morton’s neuroma and not some mystery condition or misdiagnosed!
I think you will be amazed at what the research reveals about how often Morton’s neuroma is misdiagnosed and how often it is actually seen on MRI and sonography. You still have to question if the bulged bundle of nerve and fibrous tissue is the cause of your pain.
What I want you to get out of this section is this:
Even though you have evidence of a neuroma it does not mean the pain is coming from the neuroma and it doesn’t mean you still cant avoid surgery by opening some additional space for what ever is being pinched causing the pain. I do it all the time!
X-rays Are No Benefit!
The usual route for a foot injury is to take radio-graphs of the entire foot however this is not an injury and x-rays are no help determine a positive Morton’s neuroma diagnosis vs metatarsalgia (simple pain in the toes).
This is because the neuroma is a soft tissue and you usually cannot see these soft tissue neuromas on x-rays. They are best for bones and joints. A doctor may take x-rays because every case is different and it’s hard to determine if they are medically necessary without knowing all the variables in your case. It’s safe to say you cannot see a neuroma on an x-ray.
How do I know it’s not a foot stress fracture?
The Morton’s pain, foot symptoms can different from symptoms of a stress fracture in that they feel there is a ball or stone in the bones in the foot. Patients feel as if they have a bruise causing pain and swelling under the third or fourth toe or line a stone impact bruise where the bottom of the foot hurts between the second metatarsal bone and third metatarsal bone but primarily between the third toe and fourth toe and knuckle joints of the toes.
If the pain is in the second metatarsal it could be a locking of that bone. Also you would treat a neuroma almost the same way as a stress fracture so its not critical if its hard to distinguish between the two.
For more information on stress fractures of the foot, read this article I wrote:
Stress Fracture Of the Second Metatarsal – Self Help Tips to Treatment and Prevention from The Barefoot Running Doctor, click here to view
MRI or Ultrasonography?
For many soft tissue conditions, the Morton’s neuroma MRI is the diagnostic test of choice. However, for Morton’s neuroma MRI can is good for large neuromas but the ultrasonograph is best if the neuroma is less than 5 mm.
In a study of 25 patients with confirmed Morton’s Neuroma Diagnosis, 88% were picked up by the MRI scan and 96% were picked up by the ultrasonograph. Of those 4 that were missed by the MRI and caught by the ultrasonograph, 4 of 5 were smaller than 5 mm. So for smaller neuromas, the ultrasonograph may be more sensitive. (9)
Sonography is good to differentiate between a Morton’s Neuroma Diagnosis 15.2%, an inflammation of the bursa between the toes 20.5%, and just simple swelling of the toe joints 11.7%. (10)
However, just because there is evidence of a neuroma on ultrasonography, it does not mean that the pain is coming from the neuroma. So if your doctor finds a neuroma on an MRI and ultrasonography, do not assume this is where the pain is coming from and rush off for surgery. Read on!
Not All Mortons Neuromas Are Painful Conditions
_______________________________________________________________________________________
In a study, researchers did ultrasonography on 96 feet with no pain. In this observational prospective study, patients with asymptomatic forefeet (they had no foot pain!) who were seen by two foot and ankle surgeons for unrelated mid- or hind foot pathology were examined clinically and sonographically for the presence of interdigital nerve thickening (a fibrous neuroma). (11)
Fifty-four percent of the volunteers (26 of 48) had sonographic nerve thickening and in 17 cases (35.4%) enlarged nerves were found bilaterally. (11)
Ultrasound, even in highly skilled hands, has a high rate of incidental finding of an asymptomatic inter-digital nerve enlargement (painless Morton’s neuroma), which can lead to a false diagnosis of a Morton’s neuroma. Sonographic evidence of Morton’s neuroma per se is unreliable unless it is correlated with an equivocal clinical examination. Clinical examination is still the gold standard for the diagnosis of a Morton’s neuroma. (11)
The physical exam done by someone who has reversed the symptoms of metatarsalgia where there was evidence of a Morton’s neuroma is your best physician for this.
If you go to a surgeon, what are you more likely to get? Surgery So if you go to a surgeon and he recommends surgery you should not be surprised.
While more research has been conducted since these reviews, Morton’s neuroma continues to be a complex condition with a wide variety of conservative and surgical interventions.
_________________________________________________________________________________________
The Typical Conservative Standard Treatment Protocol For Those Who Evaluate And Treat You As A Lever Mechanism
The pain caused by Morton’s neuroma is typically associated with standing activity and may be linked to wearing heels or tight shoes that compress the toe box. (12)
This is normally what doctors quote as the cause of Morton’s neuroma. If this is what they think the cause is then they are limited to changing your footwear, standard physical therapy, drugs and surgery.
There are three stages to this lever method treatment approach, which involve progressively more invasive and expensive treatment approaches.
1. The first stage consisted of
- Patient Education
- Footwear Modifications and
- Metatarsal Inflammation Relief with Physical Therapy (13)
2. The second stage consists of a steroid/local anesthetic injection into the affected interspace.
note; Stage one and two conservative treatments include footwear changes, steroid injections, physical therapy, and topical or NSAID pain reliever.(13)
3. The third stage is surgical excision of the inflamed interdigital nerve. (13)
What is interesting is 79% got better even with this very weak treatment approach. With this course of care, (21%) of the patient’s eventually required surgical excision of the nerve (13).
Just think how many may more of the 21% would have avoided surgery with a more aggressive treatment approach outlined later in this article.
Stage 1. Typical Footwear Modifications for Morton’s Neuroma
Conservative measures such as footwear modification and targeted injection of the hot spot are attempted before considering surgical intervention. (14)
The usual patient education varies depending on the depth of knowledge of the physician, how much time he or she has to educate you and the variables in your case. You may be asked to lose weight, don’t stand a lot and maybe some instructions on how to walk with less stress on your toes.
The typical footwear recommendations they make are:
- Do not to wear pointy toed or narrow toed shoes.
- Do not wear high heel shoes.
- Wear footwear that is of a soft material. I disagree with this!
- Get custom fit orthotics. I disagree with this!
I never recommend orthotics!
I never recommend a softer material for footwear!
(I explain this later)
Stage 2. Steroid/Local Anesthetic Injection for Morton’s Neuroma
Some doctors have such little faith in physical therapy, footwear modifications etc that they just recommend an injection into your foot right away the first day.
A single ultrasound-guided corticosteroid injection resulted in generally short-term pain relief for symptomatic Morton’s neuromas. The effectiveness of the injection appears to be more significant and long-lasting for lesions smaller than 5 mm. (3)
Ultrasound guided alcohol ablation of Morton’s neuroma may offer an alternative to surgery. In this study, 32% had complete resolution of pain, 66% improved but 20% went on to have surgery because of continuing pain (1)
After doctors see that conservative measures fail, surgical treatment can be indicated.
If all you had was injections before surgery you haven’t done all you can to treat this condition to prevent surgery.
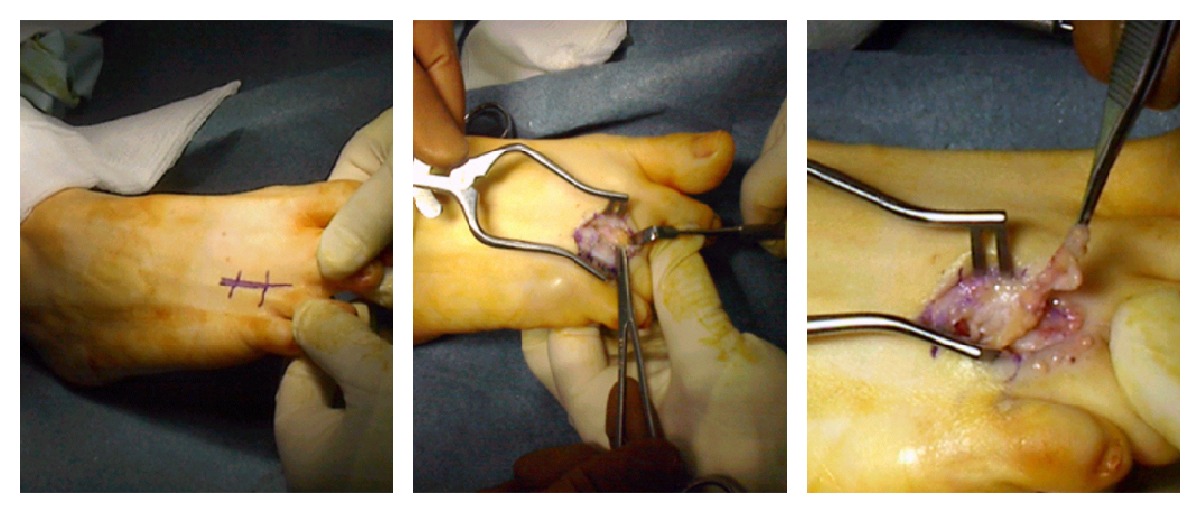
Stage 3. Surgical Excision Of The Morton’s Neuroma This is what the surgery looks like
There are two approaches to surgery to neuroma removal. There is the plantar approach and the dorsal approach.
The Plantar Approach – The plantar approach neuroma removal, can leave a painful scar on the weight bearing area; hence, some prefer the dorsal approach. (16)
The Dorsal Approach – neuroma removal is associated with better rehabilitation and less scar problems. There can be residual numbness after surgery. (16)
Most studies reveal the outcome of Morton’s neuroma excision in the treatment of metatarsalgia with a postoperative success rate of 80 – 90%.
After neuroma excision, numbness in the web space postoperative is very common but most patients are unaware of the sensory loss.
After neuroma excision surgery you could be left with a stump neuroma. A stump neuroma is a stump from a severed nerve. In some patients it causes no symptoms but with others it is extremely painful.
Keh et al. who reported a 93% long-term subjective relief from neurectomy (surgically remove the nerve)
However, the authors report that many patients complain of some residual discomfort in the region of the surgery and 70% still have some degree of footwear restriction. (17)
After surgery can I wear my heels again? Most likely, NO!
So many ladies think that once they operate to remove the neuroma they can eventually go back to the high heels again. Not so!
Footwear problems in patients may affect the outcome of neuroma removal surgery in spite of providing good pain relief. In our series, the majority (71%) had problems wearing fashionable shoes even though they were happy with the surgery. Only 29% of patients had no footwear restriction (2)
Some women resist footwear modifications or the footwear modifications of any kind. In my opinion of those I have seen where the footwear modifications were a softer shoe with an orthotic make the overall mechanics of their condition were worse.
I feel the footwear I am recommending is more effective because of the common sense reasoning behind it and because more there are more attractive style options to choose from with these recommendations.
A big applause from the shoe fan-addicts
Surgeons don’t want to admit that the surgery for Morton’s Neuroma does not always work 100% of the time!
The excision of plantar neuromas is not always successful. Publications show failures as high as 14–21%. (18)
These are the studies the surgeons do not want published. Not all studies get to the public for obvious reasons.
Do you think a clinic would publish a study with poor outcomes? Who would recommend their center if they published a study saying they had poor outcomes?
If after surgery you still have pain, what is the course of care for now?
Wasn’t surgery the LAST resort?
Spinal Cord Stimulator? I call this a radical option!
Spinal cord stimulators are used when all avenues of controlling chronic debilitating pain are exhausted. It is like a tens unit that is implanted in the abdomen which has wires that run up inside your spinal cord and deliver a current to the cord area. The patient can increase or decrease the impulse from a remote they carry around with them.
Usually these stimulators are implanted when patients have a failed back surgery syndrome. Doctors rationalize this surgery because the alternative is prescription drugs, most commonly narcotic painkillers. Because patients tend to increase the dosage as years go by the risk for overdose is greater.
I had 2 patients that had spinal cord stimulators surgically implanted in their bodies. Interesting enough, the patients had to have a psychological exam before the surgery to see if they could handle the stimulator permanently implanted in their spinal cord area.
After care at Team Doctors, because of the relief they had from the treatment approach, both patients decided to have these stimulators surgically removed.
However, in one study, SCS immediately abolished pain of the Morton’s neuroma and the patient was able to perform her normal daily activities within 1 month. (19)
The Team Doctors Human Spring Model and Approach to Mortons Neuromas
The cause and development of Morton’s Neuroma remain controversial. (20)
Although the pathology of Morton’s neuromas is understood the development or causes of Morton’s neuroma are less agreed upon.
Why?
Because doctors cannot agree on the cause of Morton’s Neuroma it makes it difficult for physicians to treat this common injury until it is too late, requiring surgery.
I explain why in this post…
What causes the abnormal nerve to become inflamed between the 3rd and 4th metatarsal heads that leads to Morton’s neuroma?
The first thing we have to understand is that chronic trauma has been proposed as possible factor in the cause of thickening of the nerve and pain described as Morton’s neuroma. (20) The nerve can thicken from a chronic inflammatory process that happens without pain.
So if we can isolate the sources of the chronic trauma and address it, we may be able to tone down the inflammation enough to reduce the pain thus save you from unnecessary pain and suffering and importantly unnecessary surgery.
This is the most sensible plan!
What can cause chronic trauma to the toes of the foot?
First we need to address the footwear cause of chronic trauma.
I agree with abstaining from pointy-toed shoes, narrow shoes and high heel shoes. If the toes are jammed together by the shoe then the toes will damage the nerve between them.
You MUST have a shoe with an open toe box. Don’t worry ladies, there are some really sharp shoes with open toe box styles.
I do not agree with wearing shoes with soft material. Here is why.
First, soft materials allow the foot to collapse into the material destabilizing the foot position. The pressure of the body weight can cause the foot to sink in at the ball of the foot so that there is the unequal weight distribution leading to a collapse of the toes together, increasing pressure between the toes.
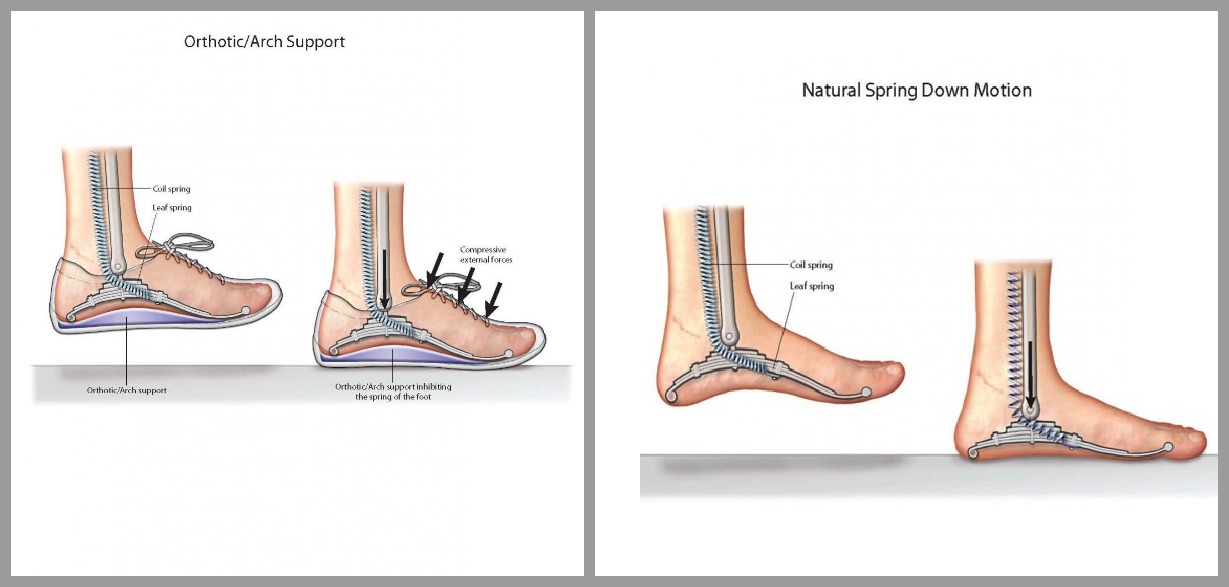
Orthotics, Inserts and Arch Supports
Apart from the etiology, increased load, which is transferred to the central metatarsals, some doctors feel Morton’s neuroma can be treated successfully with orthotic devices. (21)
I remove orthotics and take a different approach for many reasons:
We already know that the nerve is pinched from pressure on the toes. So, then further jamming the toes in the bound shoe with a space occupying shim that doesn’t allow the bones to move? How do you approach the orthotic concept when you are barefoot?
There are easier and more long-term ways to transfer the load off the sore toes without a shim (orthotic) you have to put in every shoe.
So many scientists now believe that footwear is the leading cause of deforming foot conditions. What I recommend is that children and adults walk, run and work out the barefeet as much as possible.
Zipfel, B. & Berger, L.R. Shod versus unshod: the emergence of forefoot pathology in modern humans. Conclusions: The pathological lesions found in the metatarsals of the three recent human groups generally appeared to be more severe than those found in the pre-pastoral group. This result may support the hypothesis that pathological variation in the metatarsus was affected by habitual behavior including the wearing of footwear and exposure to modern substrates. (22)
When does this scar tissue formation start?
_____________________________________________________________________________________________
There is plenty of evidence that the irritation that could be the initial stages of development of Morton’s neuroma starts in childhood.
According to the results of a study presented at the 2009 American Association Orthopedic Surgeons Annual Meeting, many young children are wearing shoes that are too small. As a result, these children may be at high risk for having serious foot deformities.
“Improper footwear is well recognized to be an extrinsic factor regarding the development of forefoot deformities. Small forefoot boxes in children’s footwear could impair toe function and proper development and promote early establishment of forefoot deformity,” said lead author Norman Espinosa, MD, of the University of Zürich.
The study, which took place in Switzerland, included 128 boys and 120 girls from age 5 to age 10. Researchers measured the children’s feet as well as their indoor and outdoor footwear to determine whether the children were wearing properly sized shoes. They also compared their footwear measurements to the sizes given on the manufacturers’ labels to see if the shoes were marked properly. Finally, they measured the angles of the children’s toes to learn whether any of the subjects were developing hallux valgus.
The study found that most of the children tested were wearing the wrong size shoes. “We defined fitting as perfect when the inner shoe length surmounted the foot length by at least 10 mm (optimal 12 mm),” explained Dr. Espinosa.
More than half (52.8 percent) of the children had outdoor shoes that were too small; 13.3 percent of children were wearing outdoor shoes that were too large for them. A similar pattern was seen with children’s indoor shoes or slippers. Six in 10 children (61.6 percent) were wearing indoor shoes that were too small; 1 in 10 (10.2 percent) were wearing shoes that were too large.
In part, the problem may arise because parents buy shoes based on the size marked by the manufacturer, perhaps without even having the child present to try on the shoe. When researchers compared the size marked on the shoe to the actual size of the shoe, they found that more than 90 percent of both indoor and outdoor shoes were smaller than the manufacturer’s marked size. Indoor shoes were almost always (97.6 percent) smaller than the manufacturer’s marked size.
“It was a truly striking finding,” says Dr. Espinosa. “The shoe sizes given by the manufacturers almost never matched with the true sizes measured by our group.”
To prevent these problems, Dr. Espinosa makes the following recommendations for parents:
- Measure the child’s feet every time new footwear is purchased.
- Consider the actual size of the shoe rather than just the number marked on the inside of the shoe or the box.
- Check for shoe fit every month or so, especially during times of a growth spurt. Many children will outgrow shoes long before the shoes wear out.
“We truly did not expect such a large percentage of incorrectly declared shoe sizes,” he says. “We now know that we should focus on parental education to help prevent early onset of juvenile foot deformity.” (23)
American Academy of Orthopedic Surgeons
American Association of Orthopedic Surgeons
______________________________________________________________________________________
What are other causes of stress on the metatarsals and surrounding tissues? What causes the irritation that leads to inflammation and scar tissue formation?
Morton’s neuroma is known to develop as a result of chronic nerve stress and irritation, particularly with excessive toe dorsiflexion.
One researcher describes it like this, Most likely a mechanically induced degenerative neuropathy that has a strong predilection for the third common digital nerve in middle aged women. (24)
Excessive motion between the third and fourth metatarsals
This explanation is made simpler by a review of the anatomy of the foot, muscles of the foot, ligaments of the foot, the foot tendons their strategic attachment and function to suspend in the foot as an integrated spring.
The answer I am providing gives us additional options for more innovative and common sense examination approaches, preventive maintenance and treatment options you and your doctor can explore.
Excessive Foot Pronation Theory
A biomechanical theory of causation involves the mechanics of the foot and ankle that excessively pronates the foot may compensate by dorsiflexion of the metatarsals subsequently irritating of the nerve between the bones.
Excessive Dorsiflexion Theory
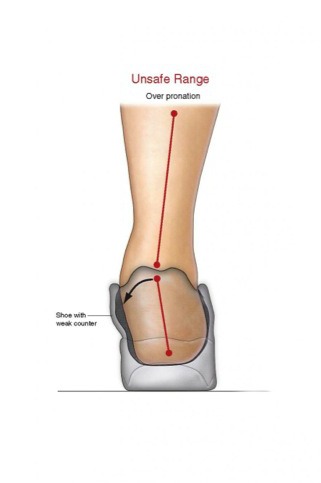
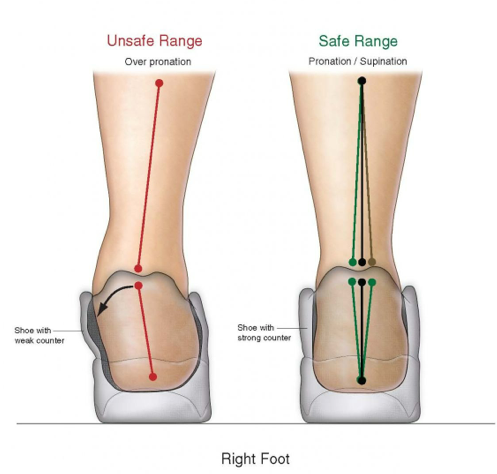
So mechanically it is most common with women who lift their toes up and those who’s foot rolls from the outside to the inside outside the safe range.
A foot that is mechanically unstable – weakness in the spring suspension system The tibialis posterior lifts and locks digit 1-3 leaving an abnormal movement between 3 and 4.
Excessive motion between the third and fourth metatarsals and metatarsal heads, the tethered third common digital nerve in the third web space, the third and fourth metatarsal heads flanking the third common digital nerve, the excessive weight bearing over use stress on the forefoot, particularly by wearing pointed and high-heeled shoes. (24)
Micro damage to the third common digital nerve causes inflammation, then scar tissue then repeats to layer scar tissue over and over again. Nerve fiber degeneration and excessive intraneual fibrous tissue formation resulting in an excessively large nerve. The enlargement can cause further trauma making it hurt more. (24)
First, you have to ask yourself this. If the cause is narrow footwear that squeezes the toes together, why is it mostly between the 3rd and 4th toes?
You would think that there would be an equal distribution of neuromas between all the toes in the foot.
The answer I am providing gives us additional options for more innovative and common sense examination approaches, preventive maintenance and treatment options you and your doctor can explore.
The answers lie in something you do every day without thinking. The answers lie in the way you walk.
Simply by closely observing your walking patterns we can see where the chronic damage is coming from. Which is causing the accumulation of fibrous scar tissue, the Morton’s neuroma and high levels of inflammation and pain in the toes, called metatarsalgia.
The Gait Evaluation – A more Thorough Examination
Videotape your walk—-
_____________________________________________________________________________
Allow me to introduce you to your human spring.
What is the difference between an intact or locked spring?
- When your spring mechanism is intact, you spring off the ground.
- When your spring mechanism is locked, you bang into the ground!
The natural spring mechanism is integrated into all 7 floors of the human body.
Essentially, the human body is a giant human spring. The body is a giant spring with 7 floors of springs:
- The arch
- The subtalar joint
- The ankle mortise
- The knee
- The hip
- The spine
- The head-neck
There are two mechanisms that allow the body to function as a spring:
- The configuration of the arch with the 26 bones and the ligament attachments.
- All 33 joints must have complete inner-joint mobility for the foot to roll from the outside to the inside without stress on any of the metatarsals.
- The spring suspension system which is composed of the muscles and tendons that attach on the under surface of the arch.
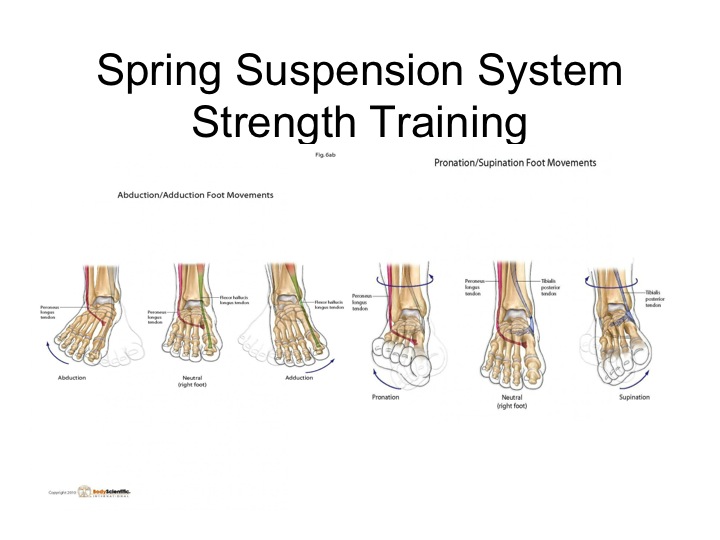
- The balance of strength in your suspension system muscles determine if your foot rolls within the safe range between rolling from the outside (supination) to the inside (pronation)
- The muscles that prevent over pronation and over supination of the foot consist of the tibialis posterior, tibialis anterior, peroneus longus, and peroneus brevis.
The strength of these supination and pronation spring suspension muscles and tendons are not covered much in bodybuilding or fitness magazines, training routines etc. but of all the muscles, in fact these are THE most important muscles in the body to work.
Why?
- These muscles suspend your foot as a leaf spring so it can bounce your body off the ground instead of bang your body into the ground.
- They store FREE elastic energy when your mass impacts the ground when they stretch. This storage of energy is what allows your body to move more efficiently as a spring mechanism rather than an inefficient lever mechanism.
These muscles, which I also refer to the pronator supinator cuff muscles, maintain the foot and lower limb in the safe range between supination and pronation.
When your foot lands it absorbs the force of the impacts two ways:
- It loads the impact force in the arch mechanism
- It rolls the impact force gradually from the outside to the inside.
The Tibialis Posterior Muscle (below) (blue tendon) This is the tibialis posterior (blue tendon) that supports the first metatarsal-cuneiform, second and third. You can also see the tibialis posterior (blue tendon), which attaches at the mid-arch at the first second and third metatarsal cuneiform joints where the spring action happens on impact.
What I have found consistently in patient after patient is a weakness in the tibialis posterior muscle. When it is weak it cannot stop the foot from over rolling into an unsafe position. When this happens the arch drops and locks in the first, second and third metatarsal cuneiform joints.
If this joint area is stiff or locked then the tibialis posterior cannot contract maximally against this joint. It’s impossible if the joint is locked. I find this muscle to be the weakest of the cuff.
When the persons walk compensates for this arch collapse drop and lock the patient has to roll the foot outward (toe out) to roll the foot around the locked arch area the foot rolls over the tibialis posterior tendon.
This abnormal stress on the tendon leads to a painful spasm of the tibialis posterior muscle-tendon that further compresses the first, second and third metatarsals together. (see blue tendon attachment)
Spasms in the muscles that cross a joint or two joints cause the joints to become compressed and when we apply this understanding to the human spring model, spasms cause a preload internal compressive force on the human spring. This preload internal compressive force reduces the overall force of impact capacity you can load into the spring mechanism.
- When your spring mechanism gets weak your spring mechanism collapses into a lever mechanism.
- When it collapses, the brain senses the abnormal movement patterns of walking as a lever and tries to protect you from the over use stress and strain by tripping spasms.
- Spasms compress the spring further.
Why is there hypermobility between the 3rd and 4th metatarsals?
If you look at the attachment of the tibialis posterior (blue), the tendons attach strategically on the first metatarsal bone, second metatarsal bone and third metatarsal bone and not the fourth metatarsal bone or fifth metatarsal bone.
The fourth and fifth metatarsals are not controlled by this tendon. They typically remain freely moving. In fact they must move more to make up for a lack of movement in the first second and third metatarsals.
When you have locking of the second and third toes at the arch joint spring (metatarsal-cuneiform) joints the foot can no longer push off straight with the second toe pointing towards the target.
The way the foot compensates for this locking is when you point the foot out like a duck walk or slew foot so you can roll around the locked joint.
So you have a complex of three metatarsals that are locked or stiffer than normal and between the 3rd and 4th metatarsals an excessive motion.
One study stated the cause of the neuroma fibrous formation was from an increased load transferred to the middle metatarsals on weight bearing. (26)
Any motion of a joint or complex of joints outside its normal range lead to abnormal movement patterns that can cause stress and strain, wear and tear, widespread silent inflammation, which starts as an invisibly swollen foot, which can lead to scar tissue development and later painful inflammation and a visibly swollen foot.
This excessive motion is what I feel causes the excessive irritation to the nerve that leads to the accumulation of fibrous scar tissue formation.
Foot Lock
When your body impacts the ground, the force of the impact is spread across 33 joints of the foot and ankle.
I do what is called motion palpation of all 33 joints of the foot to screen for any locked joints that could be preventing the safe and full loading of the stress of impacts into the body.
If any of these 33 joints are locked the stress of this impact will not be absorbed by the protective mechanism, the arch spring and the human spring suspension system, it will be transferred to the tissues leading to any number of impact stress related conditions:
Some call this an over use injury but in reality it is an injury where stress is not distributed evenly due to some joints in the foot locking and others moving too much.
The spring suspension system of the arch and its suspension system muscles and tendons protects your body from abnormal stress that leads to conditions When this drops and locks it creates over use stress through the entire body in a pattern that is predictable. Its just like a machine.
The over use stress on the other structures could manifest as over use injuries such as:
- Plantar Fasciitis
- Heel Spurs
- Heel Pain
- Foot Pain
- Morton’s neuromas
- Tibialis Posterior Tendon Dysfunction (see below)
- Ankle Sprain
- Shin Splints
- TFL & Illiotibial Band Syndrome
- Gluteus Medius Pain
- Lower Back Pain
- Mid Back Pain
- Neck Pain Syndromes
- Headaches
In his book, How I Got My Wiggle Back, Anthony Field talks about how his wife had chronic debilitating pain from Morton’s neuroma’s in both feet for 9 years. She had the MRI and the doctor said she needed surgery to remove the neuromas in both her feet. I treated her with this approach or 4-5 hours for 4 days and she was pain free which made the surgery medically unnecessary. (30)
So if you feel you have metatarsalgia or Morton’s neuroma from a weak dropped and locked spring mechanism then you should evaluate yourself for other conditions that may be developing up the pattern.
To think you wont get these actually does not abide by the laws of physics and nature. So more often than not you will see these conditions in your future if these abnormal mechanics are left untreated.
________________________________________________________________________________________
Also, another study determined that high heels increased pressure on the 3rd and 4th metatarsals. The aggravation and possibly the etiology of these forms of forefoot pain may be related to acute or chronic extrinsic pressure to the forefoot.
The role of non-weight bearing, compression of the metatarsal heads, weight bearing, and toe-stance (on the metatarsal heads) on the intermetatarsal pressure of the third interspace was measured in eleven asymptomatic volunteers.
Intermetatarsal pressures for
- Non weight bearing 21mm Hg
- Non weight bearing with medial-lateral compression of the metatarsal heads 21mm Hg
- Weight bearing 29mm Hg
- Toe Stance 36 mm Hg
These findings support the proposition that increases in forefoot plantar pressures convey greater pressures to the inter metatarsal space and metatarsal heads (27)
_____________________________________________________________________________________
The Combined Effect
If you look at the combination of the high heels elevating pressures between the toes in the forefoot, the rolling of the compressive force of the landings from the inside to the outside with over pronation combined with the locking of the first 3 toes and a excessively moving 4th toe you have a bigger picture of the full cause of this scar tissue formation between the toes.
Now we have a more thorough approach with more options to reverse this mechanical abnormality to reverse this condition with conservative care.
The Gait Evaluation – A more Thorough Examination
Simply by evaluating the gait (shown by example above in this post) you can watch it back advancing the movie slowly frame by frame to look for the conditions that might lead to Morton’s Neuroma below;
- Are your feet, shins and legs relaxed prior and during impact?
- At impact and while transferring the weight across the planted foot are any of the toes off the ground?
- Does your calf shake when it hits the ground (from the back)?
- Do you push or pull your body across the ground or spring your body off the ground?
- Does your foot point straight with the second toe being the pointer toe towards the direction you are going or do you point your toe outward like a duck walk?
- Is your shin, ankle and foot in alignment or do you have a weak or weak ankles? (over pronation)
- Do you walk heel-toe or land heel first? There is no spring there. The impact goes bone (heel) to bone (talus) to bone (shin) The spring suspension system is in the middle/front of the foot!
How do we correct the form and technique of your walk?
- Relax your foot on impact. Do not pull your toes up (dorsiflexion) prior to landing and as you transfer the weight onto your foot. This causes increased pressure when has been shown to increase the risk of Morton’s neuroma.
- Plant the foot with the second metatarsal toe pointing to the direction you are going. If half of the weight is on the big toe and the other half on toes 3-5 then the weight is equally distributed across the foot. This will reduce the over use stress on the third metatarsal bones and fourth metatarsal bones.
The answer is to control the over rolling at the heel which still allows the body to be protected from the impacts by the spring mechanism because there is nothing inhibiting the healthy rolling and loading of the arch mechanism.
Shoes – What are the best shoes for walking or running with Morton’s Neuroma?
If your muscles aren’t strong enough to hold the foot from rolling too far to the inside you wont be able to strengthen them fast enough to maintain them in the safe range between supination to pronation (outside foot to inside foot).
So you will have to get a shoe that prevents the over rolling. Here is where other doctors and I differ.
Many doctors insist on putting an orthotic or arch support to keep the arch from over rolling.
What already explained was that there was too much pressure on these joints causing the neuroma.
Why add another space occupying shim in the already confining shoe to potentially squeeze it down further.
If you inhibit spring movement with the orthotic the muscles cannot get stronger because you inhibit the spring loading down.
I never recommend orthotics for this purpose.
For more information I recommend viewing Tutorial #97 On Your Feet All Day? Fatigued? Achy? Over Pronation? I Recommend Footwear with Extended Medial Counters, click here
Human Spring Approach to Morton’s neuroma
I have developed a 3-step approach to restoring safer, spring loading capacity:
- Phase I – Release the spring from forces that create compressive forces on the human spring from muscle spasms.
- Phase II – Strengthen the spring suspension system muscles
- Phase III – Impact train the spring suspension system
Phase Ia Morton’s Neuroma Stretches treatment:
-
- Morton’s Neuroma Stretches – Remove restrictions from the spring mechanism in the 33 joints of the foot with stretching and mobilization of all 33 joints of the foot specifically those of the hypo-mobile (stiff or locked) digit 1, 2 and 3.
- You will be physically separating all the bones of the forefoot with the same muscle and tendon stretching and joint manipulation I do in my office to allow more room for the nerve to pass between the joints. This spreads out the stress to all the 33 joints lessening the stress on specifically (the third metatarsal and fourth metatarsal).
Dr Stoxen’s best stretches for Morton’s Neuroma, video tutorials:
Video Tutorial #84 Scissor Stretching Of The Feet
Video Tutorial #85 Stretching Great For Morton’s Neuromas And Heels
Video Tutorial #88 Stretching Of The Foot While Sitting At Your Chair
Video Tutorial #89 A Stretch To Increase The Flexibility Of Your Foot
Phase Ib – Morton’s Neuroma Deep Tissue Treatments:
-
-
- These treatments are focused on relaxing the painful spasms in the tense muscles of the spring suspension system primarily the tibialis posterior that are compressing the arch spring. Essentially you are releasing the over use stress from the metatarsals with a stiff or locked spring.
- One massage therapist noted positive results with massage to reverse a Morton’s neuroma (28) I suggest you read this article.
- When you do the deep tissue treatments below, the purpose is to release the compressive forces from your entire lower body to allow the bones to move more freely the way they were designed to move and not compressed with abnormal restrictive and excessive movements that cause inflammation and scar tissue formation between the toes.
-
View the Links below to Dr Stoxen’s self help video tutorials for Morton’s Neuroma:
Video Tutorial #78 Deep Tissue Treatment Of The Knee Popliteus Muscle
Video Tutorial #79 Deep Tissue Treatment Of The Gluteus Medius Muscle of the Hip
Video Tutorial #80 Deep Tissue Treatment Of The Subtalar Joint Of The Ankle On The Inside
Video Tutorial #81 Deep Tissue Treatment Of The Ankle (Subtalar Joint Outside)
Video Tutorial #82 Deep Tissue Treatment Under
Video Tutorial #83 Deep Tissue Treatment Above
Video Tutorial #87 Deep Tissue Of The Ankle Mortise
Watch above as Dr. Stoxen demonstrates the deep tissue treatment he uses to release the muscles under the toes. Specifically pay attention to the pain under the 3rd and 4th metatarsal. pictured is the deep tissue point.
Watch above as Dr. Stoxen demonstrates a great stretch for Morton’s Neuroma!
Probe your body with deep pressure for pain and sore ropy spasms outlined in these video tutorials.
-
-
- If you feel them treat them at the same time with the technique I recommend in the video tutorial.
- Release all preload tension on the spring for maximum safe deep loading of the spring mechanism.
- Now lets release the abnormal over use stress from the foot muscles that is causing the over use stress on the body by releasing the entire integrated spring mechanism from toe to head.
-
Manipulative Therapy
In one review of research on the efficiency of manual therapies on many different musculoskeletal disorders, the evidence was inconclusive, but favorable toward the use of manipulation and mobilization of the foot to decrease pain associated with Morton’s neuroma. (29)
We need to spread out the forces on the landings across all the toes. We also need to keep the pressure off the toes from landing the foot on the side or rolling the weight over the foot so it compresses the bones together.
I adjust the metatarsal cuneiform joints of all toes and spend approximately 10 – 30 hours stretching, doing deep tissue on compressive painful muscle spasms and manipulating patients feet to normalize the movement and mechanics.
Patients will tell you I really aggressively work on these muscles and joints the entire time and that this is a grueling process for not only the patient but for the doctor as well. In fact, patients have described this as a ‘pain exorcism’ or an overhaul, which addresses the accumulation of 40- 60 years of stiffness, inflammation and deformation of the body.
Dr. James Stoxen DC Shares About ‘THE PAIN EXORCISM in detail in his interview on BFM 89.9 The Business Station, From Kuala Lumpur, May 25, 2012, click here to listen now
You may think this is a long time to spend on treating the feet however remember that these patients have had their feet locked in a leather or rubber-binding device squeezing the toes for decades.
If you wear sandals all summer, that is 4 months or about 1,000,000 impacts with the foot in a dorsiflexed locked position as this is required to keep sandals on the feet.
Some female patients have to wear high heels every day for work and therefore are working in heels for 3 decades by their 55th birthday.
If the doctor is right that the deformities start in childhood with shoes that are ill fitting that means that by age 55 each patient has the damaging forces from between 100,000,000 – 130,000,000 abnormal impacts on this 33 joint complex to accumulate deformities and scar tissue which therefore stiffens the mechanism and scar tissue surrounding the nerves between the bones.
When they come to me the analogy is like trying to thaw out a piece of frozen steak with my bare hands. That is how stiff these feet are.
Morton’s Neuroma Exercises
Phase II and III – Strengthen the spring suspension system, primarily the tibialis posterior muscle with lever system training or strength training and later spring mechanism training with running, jumping and plyometric drills.
Treating the client’s muscular imbalances was an important step in combating compensation patterns the client had adopted to avoid painful motions of the foot.
You must develop of the spring suspension system muscles! This requires;
SPRING RESISTANCE TRAINING– Strengthen the spring suspension system muscles like a lever. Train with resistance exercises adding cuffs strapped to the foot moving it in a variety of directions such as eversion, inversion, abduction, adduction, pronation and supination.
SPRING IMPACT TRAINING – Strengthen the spring like a spring. I restore the spring suspension system muscles ability to resist impacts with barefoot drills like zigzag patterns, circular patterns, shuffle patterns as well as doing multi direction plyometric drills with graduated increased speeds starting with walking, jogging, running plyometrics.
Because we are going to release our natural spring mechanism, artificial spring protection like heavy cushioned soles wont be necessary. In fact, we should set a goal to get back to walking and running barefoot like we did as a youth.
Why?
“The inability to walk or run barefoot safely is one of the first signs of aging ” Dr. James Stoxen DC
Are we running to slow the aging process or speed it up? Then when you’re in the competition you can cheat by putting shoes on that allow for additional recoil of the elastic of the shoe!
Please read these articles which discuss the training of the body to improve impact resistance.
-
-
- Video Tutorial #12 Is Running Bad For Your Knees? How Does The Body Spring Back Safely From Impacts Of Running and Walking?, click here to view
- Tutorial #28 Self-Tests & Exercises To Reduce Over Pronation and Over Supination From Impacts During Walking and Running , click here to view
-
Can I wear high heels with Morton’s neuromas? NO!
Can I still run with Morton’s neuromas?
Hey, I have seen women run at high speeds down the street in high heels. Would I recommend it? No way!
If you cannot walk without banging into the ground you have no business running!
How do you know when it is safe to run again?
You just don’t go out and run and see what happens!
You have to videotape yourself walking, jogging and running at increased speeds, which test the impact resistance of the spring suspension system to maintain the foot and limb in the safe range.
Watch this video below of national champion taekwondo, Christian Medina and Dr Stoxen running barefoot down the street. One of our staff was in the back of an SUV videotaping through the window while another staff member was driving.
These are the snapshots taken from the video analysis.
As you can see we ran the entire run in zig-zag patterns. This forces the foot to land in positions that naturally release the 33 joints from different angles and strengthens the suspension system muscles equally from the inside and the outside.
That is how I have been able to run barefoot on solid concrete and asphalt streets without Morton’s Neuromas, shin splints or other impact related conditions.
In conclusion…
There is no one perfect approach. However, we should approach Morton’s neuromas and other conditions with logic that follow the laws of physics and nature.
I have tried my best to present to you my best recommendations based on these laws, the prevailing scientific literature and my many years of clinical experience.
You may not rush off to your family chiropractor or alternative medical center for this but I have found that conservative treatment at our chiropractic center with an integrative medical approach.
Please feel free to share your Morton’s Neuroma story in complete anonymity in the comments below. I will advise the best I can.
Thank you for sharing this article with those you feel it can help!
References – Morton’s Neuroma
1. Pasero G, Marson P. [Filippo Civinini (1805-1844) and the discovery of plantar neuroma]. Reumatismo. 2006 Oct-Dec;58(4):319-22. [PubMed]
2. Pace A, Scammell B, Dhar S. The outcome of Morton’s neurectomy in the treatment of metatarsalgia. Int Orthop. 2010 Apr;34(4):511-5. doi: 10.1007/s00264-009-0812-3. Epub 2009 May 30. [PubMed]
3. Fazal MA, Khan I, Thomas C. Ultrasonography and magnetic resonance imaging in the diagnosis of Morton’s neuroma. J Am Podiatr Med Assoc. 2012 May-Jun;102(3):184-6. [PubMed]
4. Adams WR 2nd. Morton’s neuroma. Clin Podiatr Med Surg. 2010 Oct;27(4):535-45. doi: 10.1016/j.cpm.2010.06.004. [PubMed]
5. Summers A. Diagnosis and treatment of Morton’s neuroma. Emerg Nurse. 2010 Sep;18(5):16-7. PubMed]
6. Quinn TJ, Jacobson JA, Craig JG, et al. Sonography of Morton’s neuromas. AJR. 2000;174(6):1723–1728. [PubMed]
7. Summers A. Diagnosis and treatment of Morton’s neuroma. Emerg Nurse. 2010;18(5):16–17. [PubMed]
8. Owens R, Gougoulias N, Guthrie H, Sakellariou A. Frimley Morton’s neuroma: clinical testing and imaging in 76 feet, compared to a control group. Foot Ankle Surg. 2011 Sep;17(3):197-200. doi: 10.1016/j.fas.2010.07.002. Epub 2010 Sep 17. [PubMed]
9. Fazal MA, Khan I, Thomas C. Ultrasonography and magnetic resonance imaging in the diagnosis of Morton’s neuroma. J Am Podiatr Med Assoc. 2012 May-Jun;102(3):184-6. [PubMed]
10. Iagnocco A., Coari G., Palombi G., Valesini G. Sonography in the study of Metatarsalgia, J Rheumatol 2001 Jun;28(6);1338-40 [PubMed]
11. Symeonidis PD, Iselin LD, Simmons N, Fowler S, Dracopoulos G, Stavrou P. Prevalence of interdigital nerve enlargements in an asymptomatic population. Foot Ankle Int. 2012 Jul;33(7):543-7. doi: 10.3113/FAI.2012.0543. [PubMed]
12. Peng H, Swierzewski SJ., III Morton’s Neuroma [PubMed]
13. Bennett GL, Graham CE, Mauldin DM. Morton’s interdigital neuroma: a comprehensive treatment protocol. Foot Ankle Int. 1995 Dec;16(12):760-3. [PubMed]
14. Hassouna H, Singh D. Morton’s metatarsalgia: pathogenesis, aetiology and current management. Acta Orthop Belg. 2005 Dec;71(6):646-55. [PubMed]
15. Fazal MA, Khan I, Thomas C. Ultrasonography and magnetic resonance imaging in the diagnosis of Morton’s neuroma. J Am Podiatr Med Assoc. 2012 May-Jun;102(3):184-6. [PubMed]
16. Faraj AA, Hosur A. The outcome after using two different approaches for excision of Morton’s neuroma. Chin Med J (Engl). 2010 Aug;123(16):2195-8. [PubMed]
17. Keh R, Ballew K. Long term follow-up of Morton’s neuroma. J Foot Surg. 1992;31(1):93–95. [PubMed]
18. Johnson JE, Johnson KA, Unni KK. Persistent pain after excision of an interdigital neuroma. Results of reoperation. J Bone Joint Surg Am. 1988;70(5):651–657. [PubMed]
19. Spinal cord stimulation for recurrent painful neuromas of the foot. Neurol Sci. 2011 Aug;32(4):723-5. doi: 10.1007/s10072-011-0649-6. Epub 2011 Jun 16. Messina G, Nazzi V, Sinisi M, Dones I, Pollo B, Franzini A. [PubMed]
20. Hassouna H, Singh D. Morton’s metatarsalgia: pathogenesis, aetiology and current management. Acta Orthop Belg. 2005 Dec;71(6):646-55. [PubMed]
21. Fuhrmann RA, Roth A, Venbrocks RA. [Metatarsalgia. Differential diagnosis and therapeutic algorithm]. Orthopade. 2005 Aug;34(8):767-8, 769-72, 774-5. [PubMed]
22. Zipfel, B. & Berger, L.R. Shod versus unshod: the emergence of forefoot pathology in modern humans. (The Foot: The International Journal Of Foot Science – Volume 17, issue 4 – December (2007) [PubMed]
23. Norman Espinosa, MD, American Academy of Orthopedic Surgeons AAOS Now March 2009 Issue [PubMed]
24. Wu KK, Mortons Interdigital Neuroma: a clinical review of its etiology, treatment and results. J Foot Ankle Surg 1996 Mar-Apr;35(2):112-9; discussion 187-8. [PubMed]
25. Rattray F, Ludwig L. Clinical Massage Therapy: Understanding, Assessing And Treating over 70 Conditions. Elmira, ON: Talus Incorporated; 2000. [PubMed]
26. Symeonidis PD, Iselin LD, Simmons N, Fowler S, Dracopoulos G, Stavrou P. Prevalence of interdigital nerve enlargements in an asymptomatic population. Foot Ankle Int. 2012 Jul;33(7):543-7. doi: 10.3113/FAI.2012.0543. [PubMed]
27. Holmes GB Jr. Quantitative determination of intermetatarsal pressure. Foot Ankle. 1992 Nov-Dec;13(9):532-5. [PubMed]
28. Berry K, Gonzalez P, Bowman RG. Physical Medicine and Treatment for Morton Neuroma. Medscape [PubMed]
29. Bronfort G, Haas M, Evans R, et al. Effectiveness of manual therapies: the UK evidence report. [Accessed January 24, 2012];Chiropractic & Osteopathy. 2010 18(3):1–33. [PubMed]
30. Field A., Truman G. How I Got My Wiggle Back, Wiley Publishing (2012) [Amazon.com]
Disclaimer
All content on teamdoctorsblog.com, including without limitation text, graphics, images, advertisements, videos, and links (“Content”) are for informational purposes only. The Content is not intended to be a substitute for professional medical treatment, advice, or diagnosis. Please remember to always seek the advice of a qualified physician or health professional with any questions you may have regarding any medical concerns. Dr James Stoxen DC and Team Doctors does not recommend or endorse any specific treatments, physicians, products, opinions, research, tests, or other information it mentions. Said Content is also not intended to be a substitute for professional legal or financial advice. Reliance on any information provided by Team Doctors is solely at your own risk.
- Fever: When you have a fever, your body is trying to isolate and expel an invader of some kind. Massage increases overall circulation and could therefore work against your body’s natural defenses.
- Inflammation: Massage can further irritate an area of inflammation, so you should not administer it. Inflamed conditions include anything that ends in itis, such as phlebitis (inflammation of a vein), dermatitis (inflammation of the skin), arthritis(inflammation of the joints), and so on. In the case of localized problems, you can still massage around them, however, avoiding the inflammation itself.
- High blood pressure: High blood pressure means excessive pressure against blood vessel walls. Massage affects the blood vessels, and so people with high blood pressure or a heart condition should receive light, sedating massages, if at all.
- Infectious diseases: Massage is not a good idea for someone coming down with the flu or diphtheria, for example, and to make matters worse, you expose yourself to the virus as well.
- Hernia: Hernias are protrusions of part of an organ (such as the intestines) through a muscular wall. It’s not a good idea to try to push these organs back inside. Surgery works better.
- Osteoporosis: Elderly people with a severe stoop to the shoulders often have this condition, in which bones become porous, brittle, and fragile. Massage may be too intense for this condition.
- Varicose veins: Massage directly over varicose veins can worsen the problem. However, if you apply a very light massage next to the problem, always in a direction toward the heart, it can be very beneficial.
- Broken bones: Stay away from an area of mending bones. A little light massage to the surrounding areas, though, can improve circulation and be quite helpful.
- Skin problems: You should avoid anything that looks like it shouldn’t be there, such as rashes, wounds, bruises, burns, boils, and blisters, for example. Usually these problems are local, so you can still massage in other areas.
- Cancer: Cancer can spread through the lymphatic system, and because massage increases lymphatic circulation, it may potentially spread the disease as well. Simple, caring touch is fine, but massage strokes that stimulate circulation are not.Always check with a doctor first.
- Other conditions and diseases: Diabetes, asthma, and other serious conditions each has its own precautions, seek a doctor’s opinion before administering massage.
- Pregnancy: No deep tissue work. Be aware: danger of triggering a miscarriage by strong myofascial work is greatest during the first 3 months (especially through work around the pelvis, abdomen, adductors, medial legs, or feet)